
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 3, May/June 2016
AFRICA
171
outcomes of some patients after CABG, to articulate it and to
interpret it. This should present insight into a private cardiac
surgical practice in South Africa where there is generally a
lack of published data, but also accentuate the possibility of
a spiritual gain from such an endeavour by obtaining new
wisdom.
Methods
All patients who had CABG surgery done consecutively by
one surgeon (MJS) between November 2000 and November
2012 in the Mediclinic Hospital, Bloemfontein, were included.
The information was obtained from a personal and ongoing
database. Almost all the patients were operated with conventional
cardiopulmonary bypass and cardiac arrest. The Ethics
Committee at the Faculty of Health Sciences, University of the
Free State, approved the study as part of a thesis.
Mortality was defined as death while in hospital. This is in
line with the EuroSCORE II as well as the Cleveland Clinic.
19,20
Pre-operative renal function was determined with the sMDRD
formula. Impairment was defined as a calculated glomerular
filtration rate (GFR) of less than 60 ml/l/1.73 m
2
or chronic
kidney disease stage III (CKD III).
Major postoperative morbidity as reported by the Society
of Thoracic Surgeons (STS) implies re-exploration, prolonged
ventilation (
>
48 hours), permanent stroke, renal failure and
deep sternal infection.
21
For this study, renal failure after surgery
was not defined on the basis of a doubling in serum creatinine
value, but as new dialysis. The STS has subsequently adjusted
its definitions for prolonged ventilation and renal failure.
22
All
patients who had rewiring after dehiscence of the sternum while
in hospital, as well as within six weeks after discharge, were
considered to have deep mediastinal infection. In addition,
gastrointestinal complications, postoperative bleeding, the use of
homologous blood products and length of hospital stay (LOS)
were also investigated.
Postoperative care was done by the surgeon in conjunction
with the nursing staff. In general the physicians get involved once
the patient develops multi-organ failure.
The additive EuroSCORE of 1999 was used to calculate the risk
for operative mortality for each patient.
23
Towards the end of the
study time period, the EuroSCORE II became available and was
introduced into the practice, but this was not applied to this study.
19
Statistical analysis
The statistical analysis was done by the Department of
Biostatistics of the Faculty of Health Sciences at the University
of the Free State. Results were summarised by calculating means
with standard deviations or percentiles (numerical variables), and
frequencies and percentages (categorical variables). Individual
possible risk factors’ relationship with mortality was investigated
using chi-squared or Fisher’s exact tests. Significant univariate
risk factors were included in a logistic regression.
Results
A total of 1 750 patients had a CABG done. Of these patients,
122 (7.0%) had an additional procedure (Table 1). Males were in
the majority at 76.8%, with females at 23.2%. The age range was
between 20 and 87 years old. The median age for males was 61
years and for females 64 years. Table 2 depicts a profile of this
population of CABG patients.
During hospitalisation, 53 patients (3.03%) died. A one-word
cause of death was given for each patient who died (Table
3). The expected mortality rate was 3.87% (69 patients). The
observed/expected mortality rate (O/E) was 0.78. In the original
EuroSCORE population the mortality rate was 4.80%.
23
Risk-adjusted mortality (RAM) allows individual surgeons
to compare their results within a larger group of patients.
24
The
RAM for this series was therefore 3.74% (0.78
×
4.80%), which is
less than the EuroSCORE cohort. Isolated CABG (no additional
procedure done with the CABG) had an observed mortality of
2.21% and an expected mortality of 3.63% with an O/E of 0.61.
More than a quarter (26.3%) of the patients was considered high
risk for operative mortality, i.e. EuroSCORE
≥
6.0.
Univariate analysis
The Working Group Panel on the Cooperative CABG Database
Project was used as a reference point.
25
Seven core risk factors
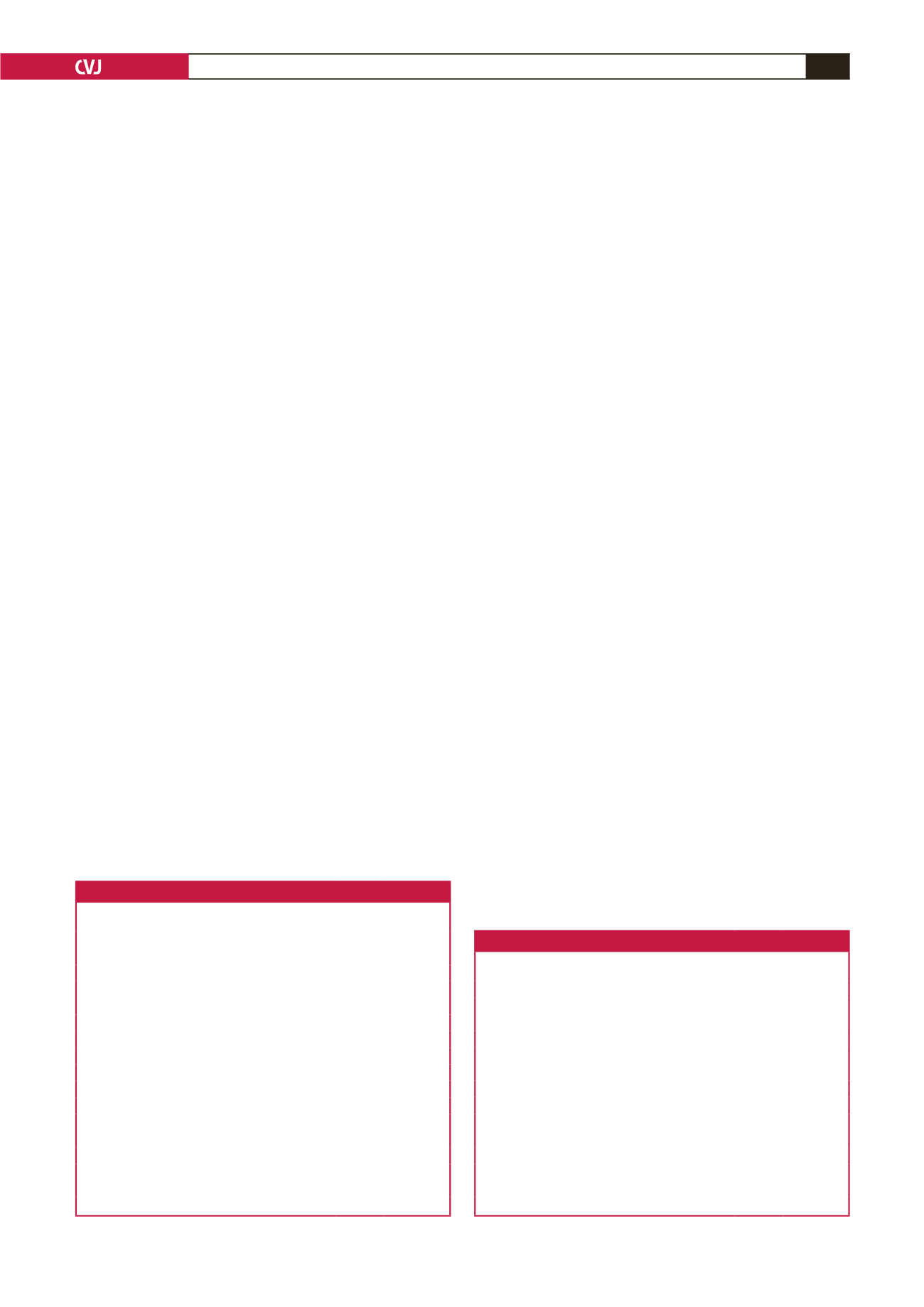
Table 1. Additional procedures to the CABG
Additional procedure
Number
Percentage
(
n
=
1 750)
Aorta dissection (intra-operative complication)
1
0.1
Aortic valve replacement
51
2.9
Aortic valve + mitral valve replacement
3
0.2
Aortic valve + mitral valve replacement + Maze
1
0.1
ASD
1
0.1
ASD + Maze
1
0.1
Biopsies for carcinoma
3
0.2
Left ventricular aneurysm
2
0.1
Left ventricular aneurysm + Maze
1
0.1
Left ventricular rupture
1
0.1
Maze
6
0.3
Mitral valve repair
15
0.9
Mitral valve repair + Maze
2
0.1
Mitral valve replacement
29
1.7
Mitral valve replacement + Maze
4
0.2
VSD (ischaemic)
1
0.1
ASD, atrio-septal defect; VSD, ventriculo-septal defect.
Table 2. Profile of CABG patients
Profile
Number
Percentage
of total
Females
406
23.2
Males
1 344
78.8
≤ 39 years
39
2.2
40–49 years
204
11.7
50–59 years
505
28.9
60–69 years
604
34.5
70–79 years
363
20.7
≥
80 years
35
2.0
Diabetes mellitus
442
25.3
Urgent (IABP/ventilator)
312
17.8
Renal impairment (CKD III)
376
21.7
Re-operation (2nd, 3rd, 4th operation)
196
11.2
Additional procedure
122
7.0
CKD, chronic kidney disease; IABP, intra-aortic balloon pump.

















