
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 1, January/February 2017
26
AFRICA
pregnant women (
p
<
0.001), respectively. Significant differences
were observed for BPWA (
p
<
0.01) and augmentation index at
75 bpm (
p
<
0.0001) between the four groups.
For BPWA, Dunn’s multiple comparison test revealed a
significant difference only between HIV-negative normotensive
and HIV-negative pre-eclamptic pregnant women (
p
<
0.01).
For augmentation index, significant differences were observed
between HIV-negative normotensive and HIV-positive
pre-eclamptic pregnant women (
p
<
0.001) and between
HIV-negative normotensive and HIV-negative pre-eclamptic
pregnant women (
p
<
0.001), as shown in Fig. 5. RHI was lower
in HIV-positive normotensive and HIV-positive pre-eclamptic
women than in normotensive HIV-negative women, although
this did not reach statistical significance (
p
=
0.1195).
Discussion
In this study, we set out to assess whether PAT (through
RHI) demonstrates endothelial dysfunction in pre-eclampsia.
The RHI was found to be significantly lower in patients with
pre-eclampsia compared to normotensive controls. Since RHI
is endothelium dependent, these results indicate that there is
indeed endothelial dysfunction in rural African women with
pre-eclampsia, therefore confirming what has been reported
in other populations. To our knowledge, this is the first report
involving rural black African women.
Endothelial dysfunction is known to be the central mechanism
in the pathophysiology of pre-eclampsia.
3
Several reports have
demonstrated that FMD is significantly reduced in patients with
pre-eclampsia when compared with normotensive controls,
18-20
confirming that pre-eclampsia is associated with endothelial
dysfunction. Although FMD measurement is still regarded
as the gold standard for assessing endothelial function in
pregnancy, it has several limitations, including the need for an
experienced sonographer, a good-quality ultrasound machine,
and the need for intra-arterial injections. It is therefore not easy
to adapt the method for use in assessing endothelial function in
large numbers of patients in a clinic setting.
We have shown in this study that the EndoPAT 2000 can
be used successfully to assess endothelial function in pregnant
subjects by measuring the RHI. Although the EndoPAT 2000
itself is a fairly expensive machine, it is less invasive, much easier
to use, does not require extensive training and it can be used to
assess large numbers of patients rapidly and reliably, even in a
clinic setting.
Although not many studies have tested endothelial function
in pregnancy using EndoPAT 2000, our results are in agreement
with the study done by Yinon
et al.
in 2006, who examined 17
women at the time of diagnosis of pre-eclampsia (mean gestation
32 weeks) and compared themwith 25 women with normotensive
pregnancies. They found that women with pre-eclampsia had
significantly lower RHI values (1.5
±
0.1 vs 1.8
±
0.1) compared
to uncomplicated pregnancies.
The results of this study with much larger number of subjects
clearly indicate that RHI, as measured using the EndoPAT, can
be used as an adjunct to blood pressure measurement in assessing
endothelial dysfunction in pre-eclampsia. However, as endothelial
dysfunction is known to precede clinical pre-eclampsia, the
important question is, can the EndoPAT 2000 be used for screening
and identifying patients before the onset of clinical pre-eclampsia?
Carty
15
followed up a cohort of patients in Scotland from the first
trimester all through pregnancy to postpartum, but did not find
any difference in RHI between women who went on to develop
pre-eclampsia and normotensive pregnancies, both at 16 and 28
weeks’ gestation. This, however, does not rule out the possibility
that RHI might still be useful in either early identification or
prediction of pre-eclampsia in larger studies, as the search for
predictors of pre-eclampsia continues in earnest.
If it were demonstrated that RHI, as measured by the
EndoPAT 2000, can be used as a predictor of pre-eclampsia, then
the test would become much more cost-effective and cheaper. A
prospective cohort study of normotensive pregnant women
recruited in the first or early second trimester and followed until
delivery is planned to determine whether RHI measurement can
be used as a predictor of pre-eclampsia.
When participants with early-onset pre-eclampsia were
compared with those with late-onset pre-eclampsia, there was
no statistically significant difference in RHI between patients
with early- and late-onset pre-eclampsia (
p
> 0.05). Although
the numbers are small, this finding suggests that endothelial
dysfunction is indeed present in both early- and late-onset
Systolic BP (mmHg)
0 20 40 60 80 100 120 140 160
Baseline pulse wave amplitude (au)
1600
1400
1200
1000
800
600
400
200
0
Fig. 4.
Relationship between systolic pressure and baseline
pulse-wave amplitude.
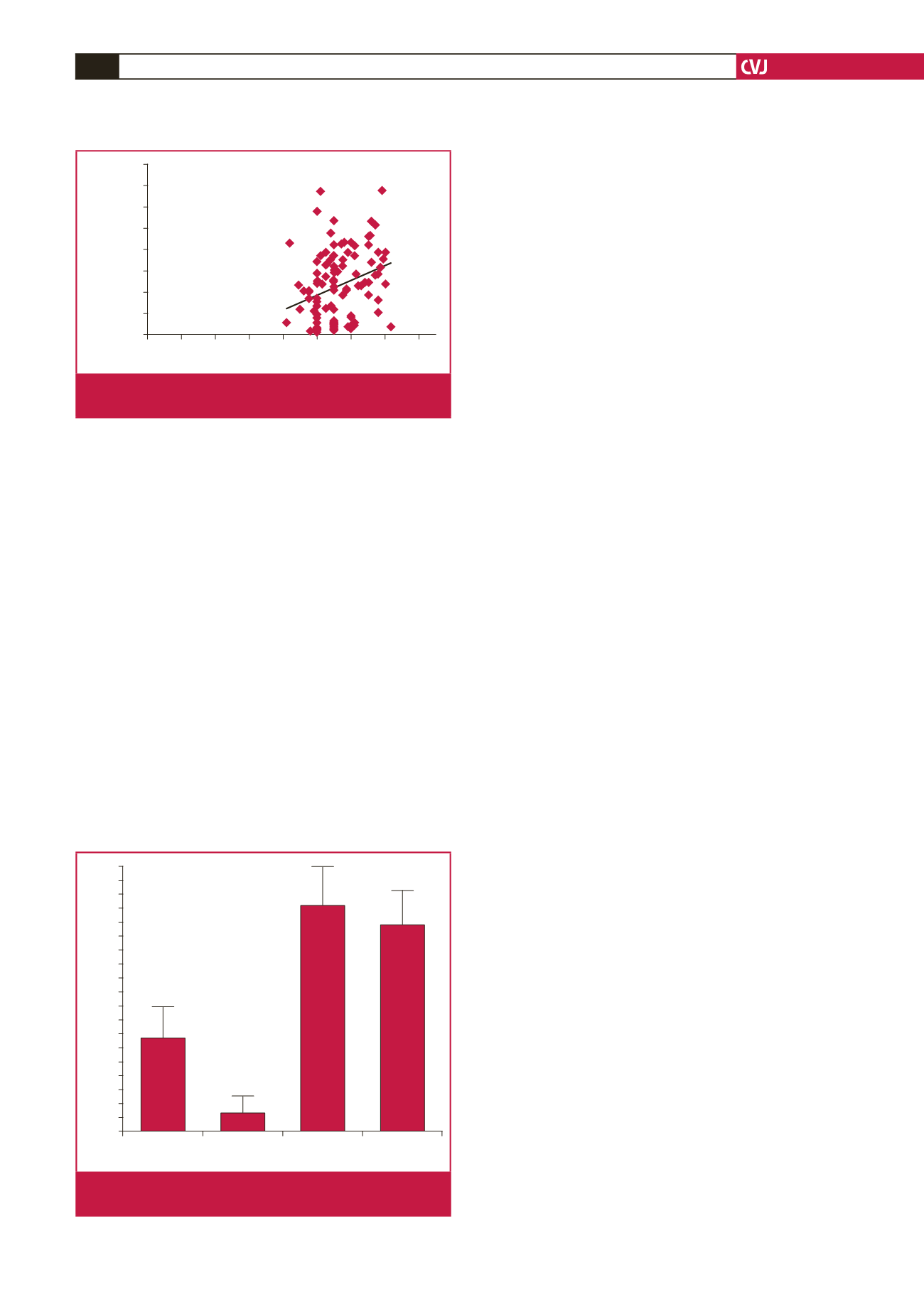
Augmentation index @ 75 bpm (%)
Normotensive
HIV+
Normotensive
HIV–
Pre-eclamptic
HIV+
Pre-eclamptic
HIV–
19
18
17
16
15
14
13
12
11
10
9
8
7
6
5
4
3
2
1
0
Fig. 5.
Augmentation index @ 75 bpm between the four HIV
groups.

















