
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 1, January/February 2017
AFRICA
21
In terms of lead function, the pacing threshold in our patients
was lower or comparable to that of CS leads.
6
We acknowledge
that the pacing threshold of epicardial leads may increase over
time due to myocardial fibrosis, and this may lead to early
battery replacement. However, there is little information on long-
term follow up of LV lead threshold in CRT. Further studies
with a longer follow up are essential.
Transvenous insertion of LV leads is currently the route of
choice for CRT. Unfortunately, its success rate is about 75 to
93%, as it is totally dependent on the inconsistent coronary
venous anatomy.
6
Although some centres do describe excellent
success rates with percutaneous leads, this does not appear
to reflect the average experience. Early and late implantation
failures are reported to occur in about 15 and 10% of patients,
respectively, with inability to cannulate the coronary sinus being
the most frequent reason for failure of lead implantation.
6
In the original reports of CRT, epicardial LV leads were
placed surgically via a left thoracotomy. These procedures
were associated with high apparent success rates.
7
One small
trial demonstrated that surgical placement of epicardial LV
leads improved symptoms as well as CS lead placement at six
months. It is not known if epicardial LV lead placement after a
failed transvenous percutaneous approach improves survival or
symptoms in the long term.
8
Puglisi
et al
.
9
reviewed their experience with epicardial LV
lead placement via a limited left thoracotomy in 33 patients with
failed transvenous lead implantation or who had experienced
early lead dislodgement. Similar to our results, they found
a larger proportion of idiopathic heart failure in patients
undergoing thoracotomy compared with patients who had
successful percutaneous CRT, and no significant reduction in
MR. They reported no surgical complications, optimal lateral
lead position in all patients, and five late deaths (15%).
Similarly, we had no surgical complications. In our study we
observed that 10 patients in NYHA functional class IV died at
the time of percutaneous implantation.
Mair
et al
.
10
described a cohort of 80 patients who had
successful LV lead implantation by thoracotomy, video-assisted
thoracoscopy, or robotically enhanced manipulation. Although
no serious adverse events were reported, technical failures
occurred in a minority of cases. Others have reported successful
CRT with video-assisted thoracoscopic surgery and robot-
assisted approaches.
11,12
Putnik
et al
.
13
reviewed the reduction in QRS complex width
(to 26.25 ms) and the increase in LVEF (12.2%). Similarly, in our
study we also described reduction in QRS complex and LVEF
improvement. We reviewed our surgical experience and found
that elective epicardial LV lead placement was associated with
improved functional status similar to that demonstrated with
transvenous LV lead placement.
2
In our study, a greater percentage of patients referred for
epicardial LV lead placement after a failed coronary sinus
approach had non-ischaemic heart failure, which suggests that
heart failure aetiology may be predictive of failure of transvenous
CRT. It is possible that a greater degree of cardiac chamber and/
or coronary sinus enlargement in patients with non-ischaemic
cardiomyopathy may limit access to appropriate pacing sites
via the coronary sinus, although this remains to be proven. By
contrast, the presence of scarred myocardium may be more likely
to lead to unacceptable pacing and sensing thresholds in patients
with ischaemic cardiomyopathy.
Our results of epicardial LV lead placement demonstrate a
clear advantage of avoiding lead-related complications and the
necessity of re-operations. Surgical LV lead placement offers
the advantage of direct access to the lateral left ventricular wall.
Direct visualisation provides an almost unrestricted opportunity
to implant the leads at the optimal target site, so that the
pre-determined lead position was achieved in all patients.
Our analysis is limited by small sample size, lack of data
regarding ventricular capture post implantation and the
retrospective design.
Conclusion
The mini-thoracotomy approach for left ventricular lead
implantation is feasible and may avoid some of the limiting
factors of transvenous procedures. Furthermore, our observed
early functional and haemodynamic improvements show a
similarity with that in the literature. This method allows optimal
lead implantation under direct vision and therefore reduces the
incidence of non-responders, resulting from sub-optimal lead
placement. We believe that with improvement in epicardial leads,
it may even have potential benefits as primary intervention
in a specific subset of patients. With further development of
minimally invasive surgical techniques and refinement in choice
of pacing leads and lead positions, epicardial left ventricular
lead placement may become a reasonable alternative for select
patients with heart failure.
References
1.
Cesario DA, Turner JW, Dec GW. Biventricular pacing and defibrillator
use in chronic heart failure.
Cardiol Clin
2007;
25
(4): 595–603.
2.
Frattini F, Rordorf R, Angoli L, Pentimalli F, Vicentini A, Petracci B,
et
al
. Left ventricular pacing lead positioning in the target vein of the coro-
nary sinus: description of a challenging case.
Pacing Clin Electrophysiol
2008;
31
(4): 503–505.
3.
Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh
E,
et al
. Cardiac resynchronization in chronic heart failure.
New Engl J
Med
2002;
346
(24): 1845–1853.
4.
Alonso C, Leclercq C, d’Allonnes FR, Pavin D, Victor F, Mabo P,
et al
.
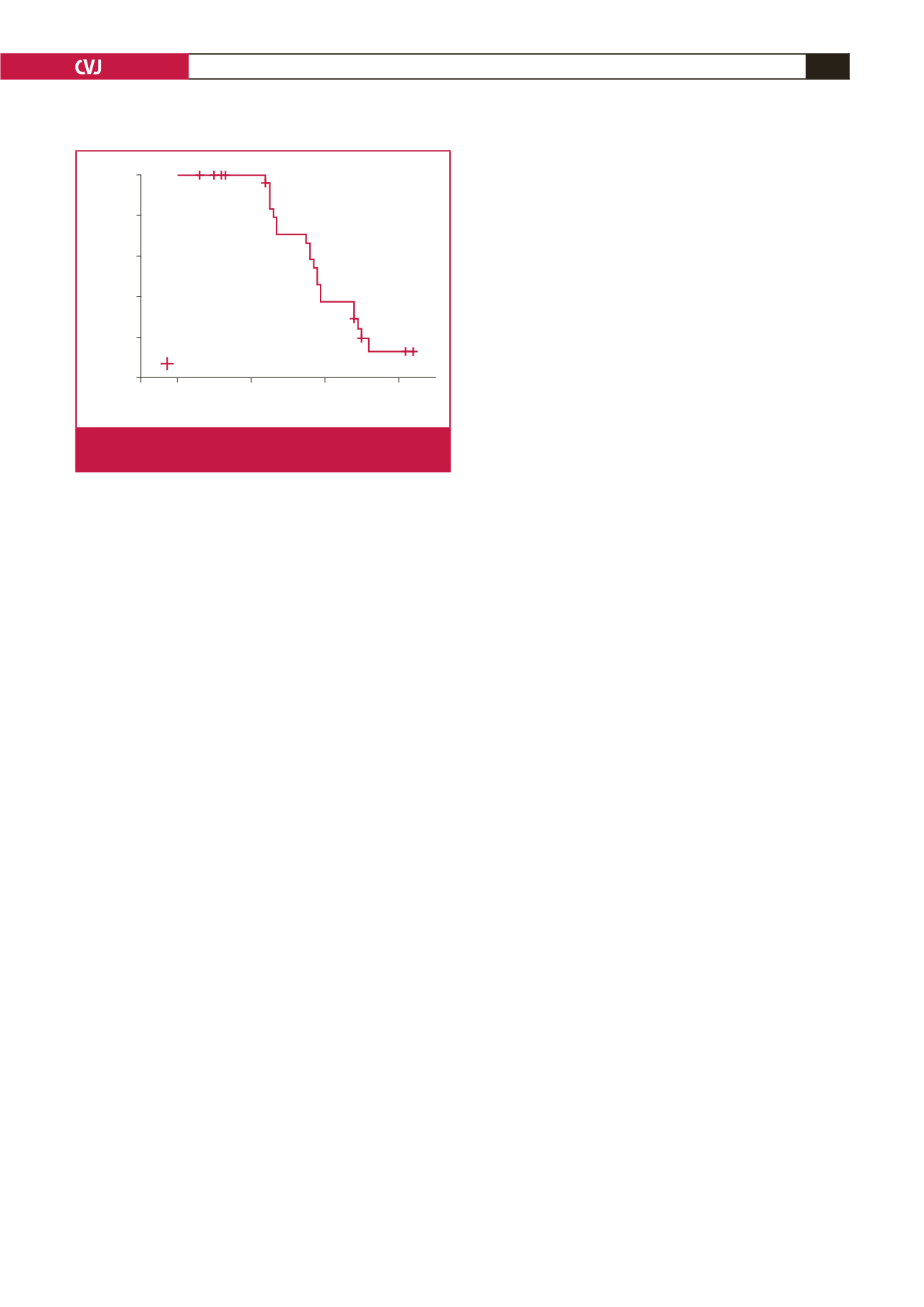
0
20
40
60
1.0
0.8
0.6
0.4
0.2
0.0
Censored
Cumulative survival
Survival function
Fig. 3.
Long-term survival following surgical left ventricular
lead placement by Kaplan–Meyer analysis (
n
=
30).

















