
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 3, May/June 2018
AFRICA
195
ECG Series
Irregular, narrow-complex tachycardia
Julian Hoevelmann, Charle Viljoen, Ashley Chin
Abstract
The correct differentiation of an irregular, narrow-complex
tachycardia has crucial implications for the therapeutic
management of these conditions. In this article we present
a differential diagnostic and treatment approach to irregular,
narrow-complex tachycardias.
Keywords:
ECG, atrial fibrillation, atrial flutter, multifocal atrial
tachycardia
Cardiovasc J Afr
2018;
29
: 195–198
www.cvja.co.zaA 54-year-old lady with longstanding hypertension and a recent
diagnosis of atrial fibrillation presented to the emergency unit
with a two-day history of palpitations and mild dizziness. This
was preceded by a few weeks of pedal oedema, with progressively
worsening dyspnoea and effort intolerance. Clinically, she was
mildly distressed with peripheral oedema, a respiratory rate of 24
breaths a minute and blood pressure of 129/84 mmHg. She had
a low-volume pulse that was irregularly irregular, with a rate of
around 120 beats per minute. The jugular venous pressure was not
elevated, but her apex beat was diffuse and minimally displaced.
On auscultation she had heart sounds of variable intensity, but no
murmurs. Her chest had soft crackles in the bases.
Echocardiography revealed a non-dilated left ventricle with
signs of concentric left ventricular hypertrophy (LVH) and
impaired left ventricular (LV) function [LV ejection fraction
(LVEF) of 40%]. The left atrium was dilated and there was mild
mitral regurgitation (MR). She had normal pulmonary artery
pressures and right ventricular (RV) function.
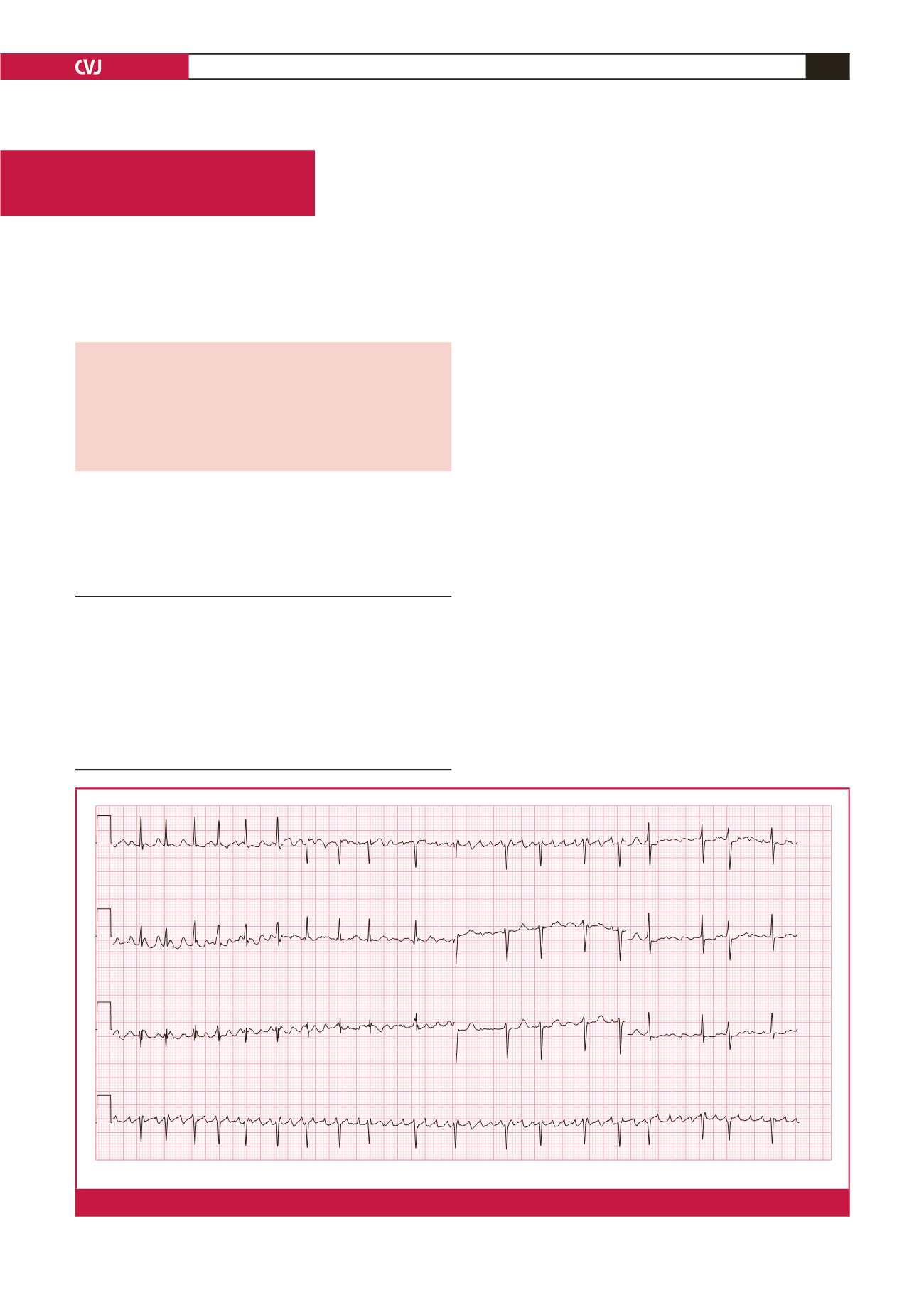
Her ECG (Fig. 1) showed an irregular, narrow-complex
tachycardia. Very rapid, continuous and variable atrial activity
was seen. The question was raised whether this ECG could be
in keeping with ‘course’ atrial fibrillation or atrial flutter with
variable block (Fig. 2). Careful inspection of the atrial activity
revealed that there was subtle variation in rate, amplitude and
Hatter Institute for Cardiovascular Research in Africa,
University of Cape Town, South Africa, and Hannover
Medical School, Department of Cardiology and Angiology,
Hannover, Germany
Julian Hoevelmann
Division of Cardiology, Groote Schuur Hospital and
University of Cape Town, South Africa
Charle Viljoen, MB ChB, MMed, FCP (SA),
charle.viljoen@uct.ac.zaAshley Chin, MB ChB, FCP (SA), MPhil
I
II
III
aVR
aVL
aVF
V1
V2
V3
V4
V5
V6
V1
dollie, shireen
ID:026928135
22-JAN-2018 10:20:40
GROOTE SCHUUR HOSPITAL
Atrial fibrillation with rapid ventricular response with premature ventricular or aberrantly conducted complexes
ST & T wave abnormality, consider inferior ischemia or digitalis effect
Abnormal ECG
25mm/s 10mm/mV 150Hz 7.1.1 12SL 239 CID: 1
Referred by:
Confirmed By: DOC UNCONFIRMED
BPM 117
Vent. rate
ms
*
PR interval
ms
102
QRS duration
ms
QT/QTc
364/507
-58
4*
P-R-T axes
Female Caucasian
Room:
Loc:34
Technician:
Test ind:
Page 1 of 1
EID:9 EDT: 14:52 24-JAN-2018 ORDER:
Fig. 1.
The 12-lead ECG with coarse atrial fibrillation, which could easily be mistaken for atrial flutter.

















