
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 2, March/April 2019
AFRICA
105
Mean (SD) initial heart rate was 85.9 (15.4) beats per minute
(bpm), with last achieved mean heart rate 71.7 (11.0) bpm. The
majority of patients were on guideline-recommended heart
failure therapy. For example, 95.8% of patients were prescribed
angiotensin converting enzyme (ACE) inhibitors and 89.8% were
prescribed spironolactone (Table 2).
At their last clinic visit, 489 patients (97.8%) were prescribed
and tolerating a beta-blocker. Patients were stratified into
categories according to target doses of beta-blocker achieved
(Table 1). Twenty-six patients (5%) were on atenolol, as they
collected their prescriptions from peripheral clinics where this
was the only beta-blocker available to them. Carvedilol was
used by 463 (92.6%) patients, while none were on metoprolol or
bisoprolol because these were not available in CMJAH during
the study period.
In 59.8% (
n
=
299) of patients a target dose was achieved,
while in 28.0% (
n
=
140) a moderate dose was achieved, and only
5.4% (
n
=
50) of patients received a low dose of beta-blockers
(Fig. 1). Reasons for intolerance, defined as no or low doses (
<
50% of target dose), and reasons for not achieving target dose
are detailed in Table 3. Conventional reasons for clinician beta-
blocker caution, such as bronchospasm or breathlessness (
n
=
7;
1.4%), peripheral arterial disease (
n
=
0), syncope (
n
=
3; 0.6%),
cardiac decompensation (
n
=
4; 0.8%) and hypotension (
n
=
2;
0.2%) were uncommon.
Of patients who were not at target beta-blocker dose,
approximately 10% were still in the up-titration phase at the
end of the study period, while in 5% (
n
=
25) no reason was
determined. Bradycardia was the most common reason for lack
of up-titration to target dose. Of the 201 patients who did not
achieve target dosing, 51.7% were at target heart rates.
18
There were no statistically significant correlates for intolerance
in terms of ethnicity, cause of heart failure or presence or absence
of concurrent treatments. A history of asthma (
p
=
0.021) and
a diagnosis of hypothyroidism (
p
=
0.009) were independently
correlated with beta-blocker intolerance.
Patients were deemed to be ivabadrine ‘suitable’ if they were
in sinus rhythm, with a LVEF
<
35% and a resting heart rate
of ≥ 70 bpm after appropriate up-titration of a beta-blocker.
7
Of the 500 patients who were initially assessed, 137 met this
criterion (27.4%). After excluding patients with New York Heart
Association class I symptoms, only 53 (10.6%) were deemed to
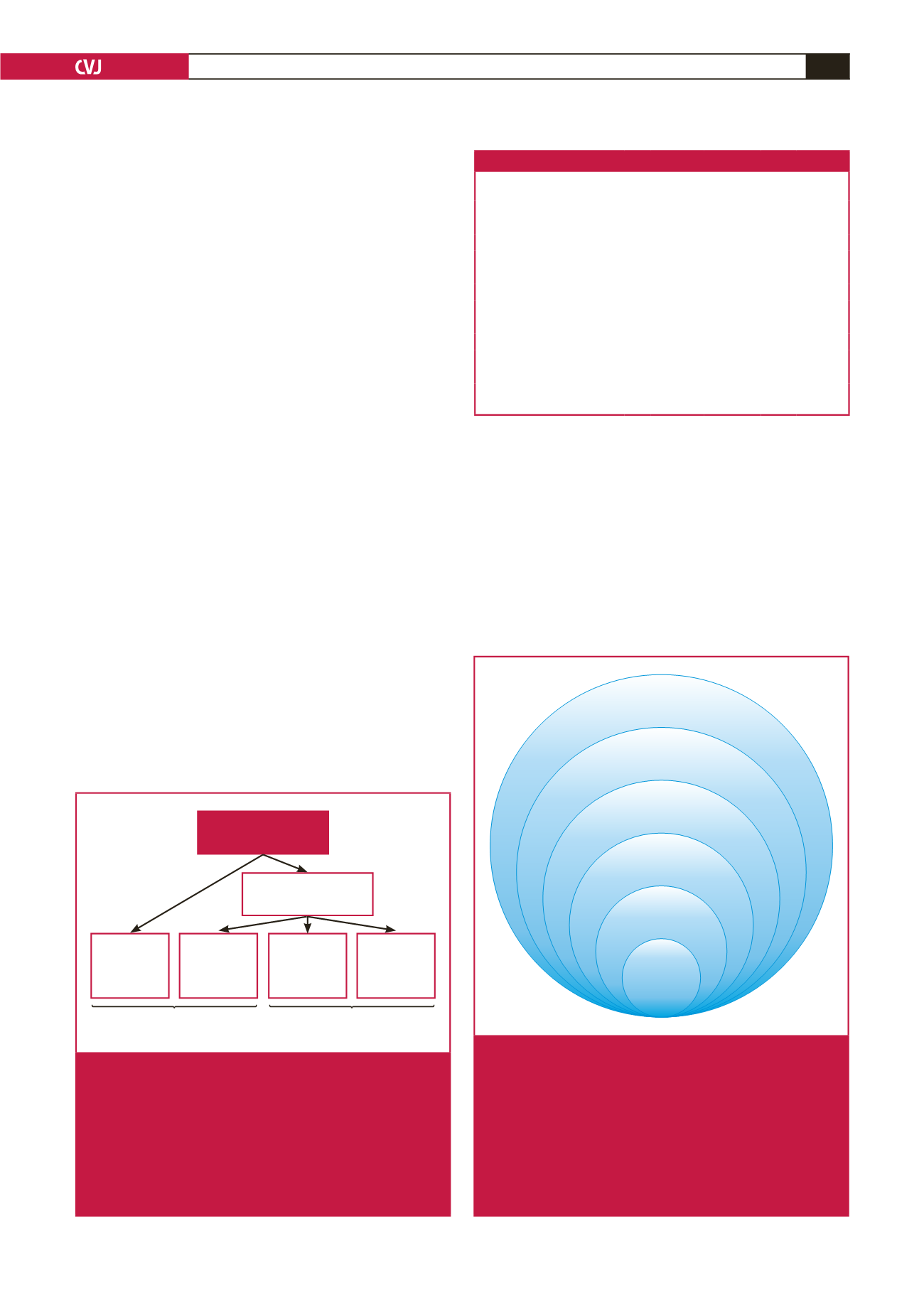
be ivabadrine suitable (Fig. 2).
The ivabadrine-suitable subgroup at enrolment had a lower
Patients with HFrEF
n
= 500
Taking a beta-blocker
n
= 489 (97.8%)
No BB
n
= 11
(2.2%)
Low-dose
of BB
n
= 50
(5.4%)
Moderate
dose of BB
n
= 140
(28%)
Target dose
of BB
n
= 299
(59.8%)
Beta-blocker “intolerant”
n
= 61 (12.2%)
Beta-blocker “tolerant”
n
= 439 (87.8%)
Fig. 1.
Study flow diagram showing categorisation of patients
according to use of beta-blocker and beta-blocker
dosage at the end of the study period. Patients on
beta-blocker at the end of the study period were
categorised into ‘low’, ‘moderate’ or ‘target’ dose of
beta-blocker therapy. Patients who were on only a low
dose of beta-blocker therapy or no beta-blocker thera-
py were termed ‘beta-blocker intolerant’. HFrEF: heart
failure with reduced ejection fraction. BB: beta-blocker.
Ivabradine
suitable
(
n
= 53)
NYHA II–IV
(
n
= 80)
HR > 70
(
n
= 165)
EF < 35%
(
n
= 314)
Sinus rhythm
(
n
= 436)
LV impairment
(
n
= 500)
Fig. 2.
Identification of patients who may have qualified for
further rate-reduction therapy. Patients with heart
failure due to impaired left ventricular function (LVEF
<
50%) constituted the entire study population. Of the
500 patients with heart failure and reduced EF, only
53 would have qualified for further heart rate-reduction
therapy with ivabradine on the basis of being in sinus
rhythm, having a LVEF
<
35%, having a heart rate of
> 70 bpm and being in NYHA class II–IV heart failure.
LV: left ventricular; EF: ejection fraction.
Table 3. Reasons for not achieving target beta-blocker dosage
No
BB
Low-dose
BB
Moderate-
dose BB Total
%
(
n
=
500)
Syncope
1
2
0
3
0.6
Hypotension
0
0
1
1
0.2
Cardiac decompensation
0
0
4
4
0.8
Raynaud’s phenomenon/ PAD 0
0
0
0
0
Bradycardia
6
22
78
106
21.2
Bronchospasm/breathlessness
3
2
2
7
1.4
Fatigue
0
3
2
5
1.0
Non-compliance
0
4
12
16
3.2
Up-titration phase
1
12
21
34
6.8
Unknown
0
5
20
25
5.0
Total
11
50
140
201
40.2
BB
=
beta-blocker; PAD
=
peripheral arterial disease. The patients were on no
BB, a low dose of BB or a moderate dose of BB at the last visit.

















