CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 4, July/August 2019
AFRICA
225
groups, which suggested that perindopril treatment did not have
a significant effect on these variables.
We also analysed the changes in the echocardiographic
parameters from baseline until the end of the follow-up period.
For this purpose, we compared the differences in the values
recorded at the end of the follow-up period between the two
groups. As a result, we found that only the change in the A
′
(sep)
velocity parameter was statistically significant. In the perindopril
group, the A
′
(sep) velocity increased, whereas it decreased in the
control group. During the study we observed 0.61 cm/s increase
in A
′
(sep) velocity in the perindopril group and a decrease of
0.28 cm/s in the control group (0.61 vs –0.28 cm/s, 95% CI:
0.039–1.748,
p
=
0.04). The increase in Sm (sep) velocity in the
perindopril group also reached near significance (
p
=
0.054). The
changes observed in the other parameters were not statistically
significant (Table 4).
Secondary outcomes: At the end of the follow-up period,
the median NT-proBNP level was 150 pg/ml. In the perindopril
group, the median level was 151 pg/ml and in the control group,
it was 149 pg/ml. When the two groups were compared, the
NT-proBNP levels were not found to be significantly different (
p
=
0.688 for the comparison of the median values). NT-proBNP
levels did not change significantly with perindopril.
At the end of the follow-up period, 57 (65%) patients were in
NYHA functional class 2, whereas 31 (35%) were in NYHA class
3. When we compared the two groups, no statistically significant
difference was found in terms of the functional capacity at the
end of the study (
p
=
0.184). When we analysed the two groups to
determine the change in functional capacity during the follow-up
period, no meaningful changes in NYHA functional class were
found in either group (Table 5).
Discussion
HFpEF is a clinical syndrome that is becoming more frequently
seen as the population ages worldwide. More strikingly, its
mortality rate has not changed for decades while the mortality
rate of systolic HF has declined significantly.
21
DD is an
important component of HFpEF. Some small studies have
reported improvements in DD with some drugs such as CCBs,
aldosterone receptor blockers, ACEIs and ARBs in this patient
population.
14-17
However, no previous study assessed the effect of
perindopril on diastolic and systolic function in HFpEF patients.
In this study, we found that perindopril treatment increased
tissue Doppler septal late diastolic velocity and slightly increased
tissue Doppler septal systolic myocardial velocity in HFpEF
patients. It did not improve the E/E
′
ratio and tissue Doppler
early diastolic velocity, which are markers of increased diastolic
pressure in this population. The other diastolic parameters
did not improve with perindopril treatment. In fact, only a
few studies have reported improvements in systolic or diastolic
echocardiographic parameters in HFpEF patients. One of these
studies is the Hong Kong Diastolic Heart Failure study, which
reported improvements in E
′
and Sm velocities with ramipril
and irbesartan.
17
It is well known that both E
′
and Sm velocities
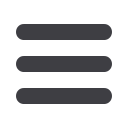
Table 3. Comparison of the echocardiographic parameters
at the end of the 11-month follow-up period
Variable
Perindopril group
(
n
= 37)
Control group
(
n
= 51)
p
-value
LA diameter (mm)
40
±
5
40
±
4
0.994
LVH,
n
(%)
11 (30)
13 (26)
0.809
LAVI (ml/m²)
25
±
6
25
±
5
0.830
M-mode EF (%)
65
±
7
64
±
6
0.669
E/A ratio
0.86
±
0.24
0.83
±
0.21 0.520
E
′
(sep) velocity (cm/s)
6.8
±
0.7
6.6
±
0.7
0.153
E
′
(lat) velocity (cm/s)
7.2
±
0.8
7.0
±
0.9
0.460
A
′
(sep) velocity (cm/s)
10.8
±
2.4
9.9
±
1.2
0.036
A
′
(lat) velocity (cm/s)
10.5
±
1.8
10.4
±
1.5
0.710
E
′
(mean) velocity (cm/s)
7.0
±
0.5
6.8
±
0.7
0.165
A
′
(mean) velocity (cm/s)
10.7
±
1.6
10.2
±
1.2
0.093
E
′
/A
′
(mean) ratio
0.67
±
0.13
0.68
±
0.11 0.628
E/E
′
(mean) ratio
11.2
±
2.4
11.6
±
2.7
0.487
Sm (lat) velocity (cm/s)
8.1
±
1.8
7.8
±
1.3
0.399
Sm (sep) velocity (cm/s)
8.5
±
2.2
7.6
±
1.4
0.025
Sm (mean) velocity (cm/s)
8.3
±
1.6
7.7
±
1.1
0.034
DD grade,
n
(%)
Grade 1
30 (81)
44 (86)
0.564
Grade 2
7 (19)
7 (14)
IVRT, mean (msn)
118
±
16
117
±
17
0.806
DT, mean (msn)
224
±
27
233
±
29
0.128
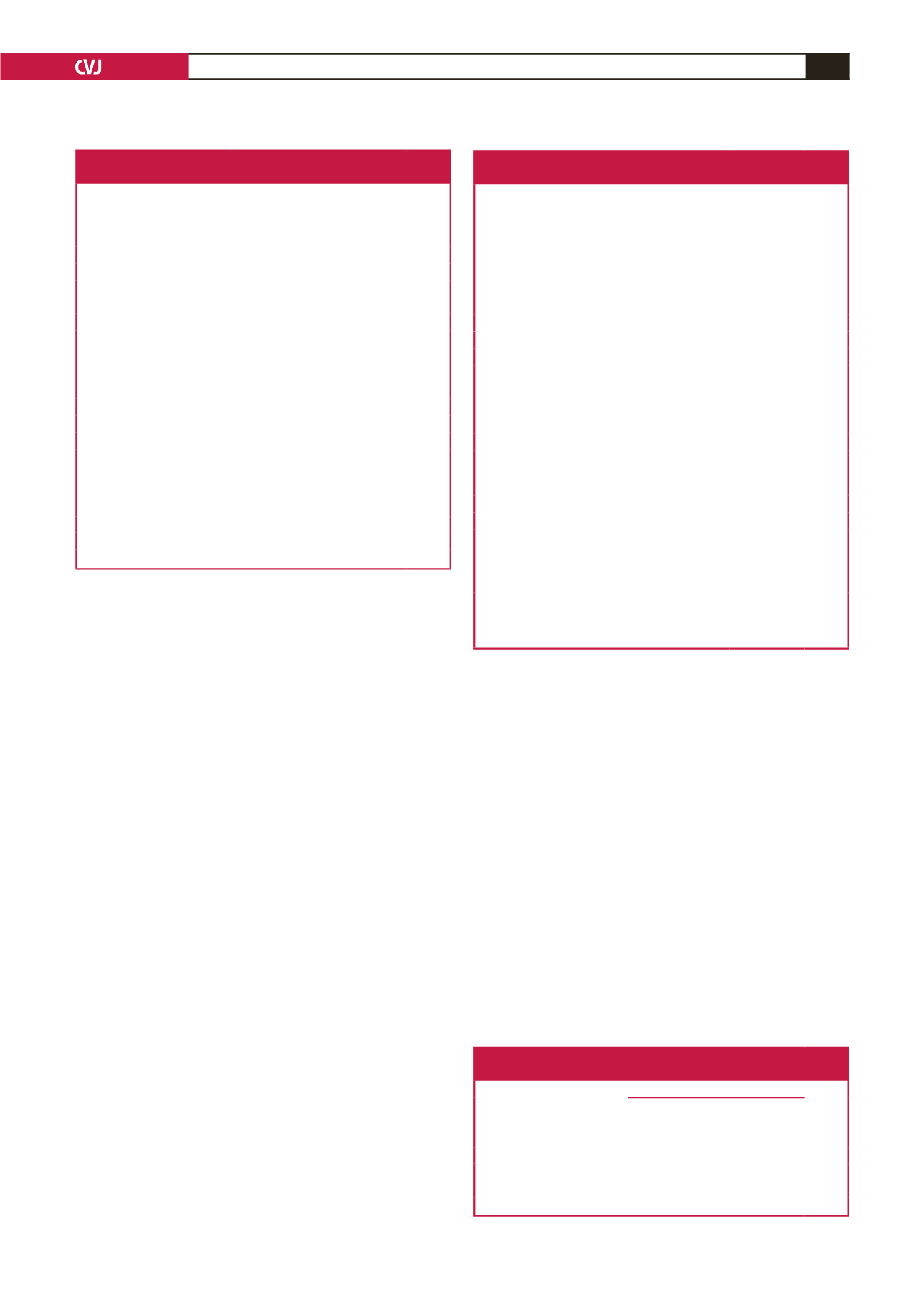
Table 4. Comparison of the change in echocardiographic parameters
during the 11-month follow-up period between the two groups
Variable
Perindopril
group (
n
= 37)
Control group
(
n
= 51)
p
-value
Change in LA diameter (mm)
0.2
±
2.0
–0.1
±
1.9 0.449
Change in LAVI (ml/m²)
0.74
±
2.77
0.55
±
3.14 0.764
Change in M-mode EF (%)
–0.8
±
6.7
–0.5
±
6.9 0.864
Change in E/A ratio
0.03
±
0.26
0.03
±
0.20 0.977
Change in E
′
(sep) velocity (cm/s)
0.35
±
0.90
0.14
±
0.83 0.253
Change in E
′
(lat) velocity (cm/s)
0.48
±
0.87
0.55
±
0.92 0.737
Change in A
′
(sep) velocity (cm/s)
0.61
±
2.04 –0.28
±
1.95 0.040
Change in A
′
(lat) velocity (cm/s)
0.21
±
2.47
0.16
±
2.04 0.921
Change in E
′
(mean) velocity (cm/s)
0.42
±
0.69
0.35
±
0.66 0.634
Change in A
′
(mean) velocity (cm/s)
0.42
±
1.54 –0.05
±
1.65 0.171
Change in E
′
/A
′
(mean) ratio
0.01
±
0.11
0.03
±
0.13 0.394
Change in E/E
′
(mean) ratio
–0.2
±
2.5
0.4
±
2.0 0.259
Change in Sm (lat) velocity (cm/s)
0.84
±
1.26
0.85
±
1.43 0.995
Change in Sm (sep) velocity (cm/s)
0.99
±
1.73
0.36
±
1.28 0.054
Change in Sm (mean) velocity (cm/s)
0.90
±
1.12
0.60
±
1.07 0.210
Change in IVRT, according to DD
grade (msn)
Grade 1
–18
±
18
–14
±
18 0.373
Grade 2
– 2
±
20
–3
±
19 0.873
Change in DT, according to DD
grade (msn)
Grade 1
–15
±
28
–12
±
21 0.660
Grade 2
–8
±
42
–10
±
32 0 295
The change in the parameters was calculated as the value at 11 months – value
at 0 months. Because the meaning of the change in DT and IVRT was different
in diastolic dysfunction grades 1 and 2, the comparisons between DT and IVRT
values were stratified according to the diastolic dysfunction grade.
Table 5. Change in NYHA functional class of the patients in the two
groups of the study at the end of the11-month follow-up period
NYHA class, 0 months
NYHA class, 11 months
p
-value
Class 2
Class 3
Group 1
Class 2
25
4
0.687
Class 3
2
6
Group 2
Class 2
28
5
0.453
Class 3
2
16



















