
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 5, September/October 2019
AFRICA
281
alirocumab dose during the parent studies. However, all eligible
patients fromHigh FH received a starting dose of alirocumab 150
mg Q2W because this study had selected patients with LDL-C
>
4.14 mmol/l at baseline. Alirocumab was self-administered by the
patient via subcutaneous injection using a pre-filled pen injector.
LDL-C levels were unblinded from week 8 to allow for
dose adjustment at the investigator’s discretion. Up-titration to
alirocumab 150 mg Q2W could occur from week 12 onwards
if LDL-C was
>
1.8 mmol/l. In addition, down-titration to
alirocumab 75 mg Q2W was possible at the investigator’s
discretion. Background treatment, including statin and other
lipid-modifying treatment, were to be maintained unchanged
unless tolerability warranted adjustment.
Site visits were performed at weeks 4, 8, 12, 24, 36, 48,
60, 72, 84, 96 and 108. During these visits lipid parameters,
liver function tests, creatinine phosphokinase, haematological
and chemistry investigations were performed. Anti-alirocumab
antibodies were assessed by the Regeneron Clinical Bioanalysis
group from serum samples, as previously described.
8
This study was conducted in accordance with the principles
laid down by the 18thWorldMedical Assembly and all applicable
amendments laid down by the World Medical Assemblies and
the ICH guidelines for good clinical practice. This clinical trial
was recorded in clinicaltrials.gov (NCT01954394).
Written informed consent was obtained before a patient’s
participation in the clinical trial and all patients were given a
copy of the signed informed consent. This clinical trial protocol
was approved by the relevant private and public sector ethics
committee. The clinical events committee was responsible for
defining, validating and classifying cardiovascular events, as well
as validating the classification of the cause of all deaths.
Statistical analysis
As this study was an open-label extension for patients from
previous studies, no calculation of sample size was performed.
Safety analyses were performed on the safety population, which
consisted of patients receiving at least one dose or a partial
dose of alirocumab in the current study. Efficacy analyses were
performed on patients receiving at least one dose or a partial
dose of alirocumab in the current study, with a baseline (from
the parent study) LDL-C value available and with at least one
LDL-C value available in the period from first alirocumab
injection in the current study to last injection plus 21 days; a
modified intention to treat (mITT) analysis.
Safety analysis [adverse events (including adjudicated
cardiovascular events), laboratory, vital signs] was descriptive,
based on the safety population. The safety analysis focused on
the Treatment Emergent Adverse Events (TEAE) period defined
as the time from the first dose of the current study to the last
dose of alirocumab plus 70 days (10 weeks).
Efficacy variables were explored through descriptive statistics
at each scheduled visit of the current study; 95% confidence
intervals are provided for percent changes from baseline and
success rate to reach targets.
Results
The study enrolled 167 South African patients at 14 sites.
Baseline characteristics and medical history for the participants
are indicated in Table 2.
All patients received treatment with lipid-modifying therapy
(LMT) at study entry (Table 3). High-dose statin and ezetimibe
use was 64.7 and 27.5%, respectively. Data specifying specific
combinations of statins and ezetimibe used during the study
were not recorded. During the OLE study, concomitant LMT
was adjusted at the investigator’s discretion.
Of the 42 patients for whom a change in statin therapy was
reported during the OLE study, 18 reported a change in statin
type, 15 reported dose adjustments in statin therapy, while nine
patients discontinued statins. The reasons provided included
adverse events, supply issues, treatment cost and other.
The mean (
±
SD) baseline LDL-C was 3.65
±
1.9 mmol/l.
Mean LDL-C level was reduced by 48.7% at week 144; mean
on-treatment LDL-C was 2.30
±
1.24 mmol/l at week 144. At
week 144, 40 of 98 patients with data available (40.8%) reached
target LDL-C
<
1.81 mmol/l and/or
≥
50% reduction from
the parent study baseline, and 64/98 (65.3%) patients reached
LDL-C
<
2.59 mmol/l. During the OLE study, calculated LDL-C
values
<
0.65 mmol/l were reported on two consecutive occasions
for four patients (Table 4, Fig. 2).
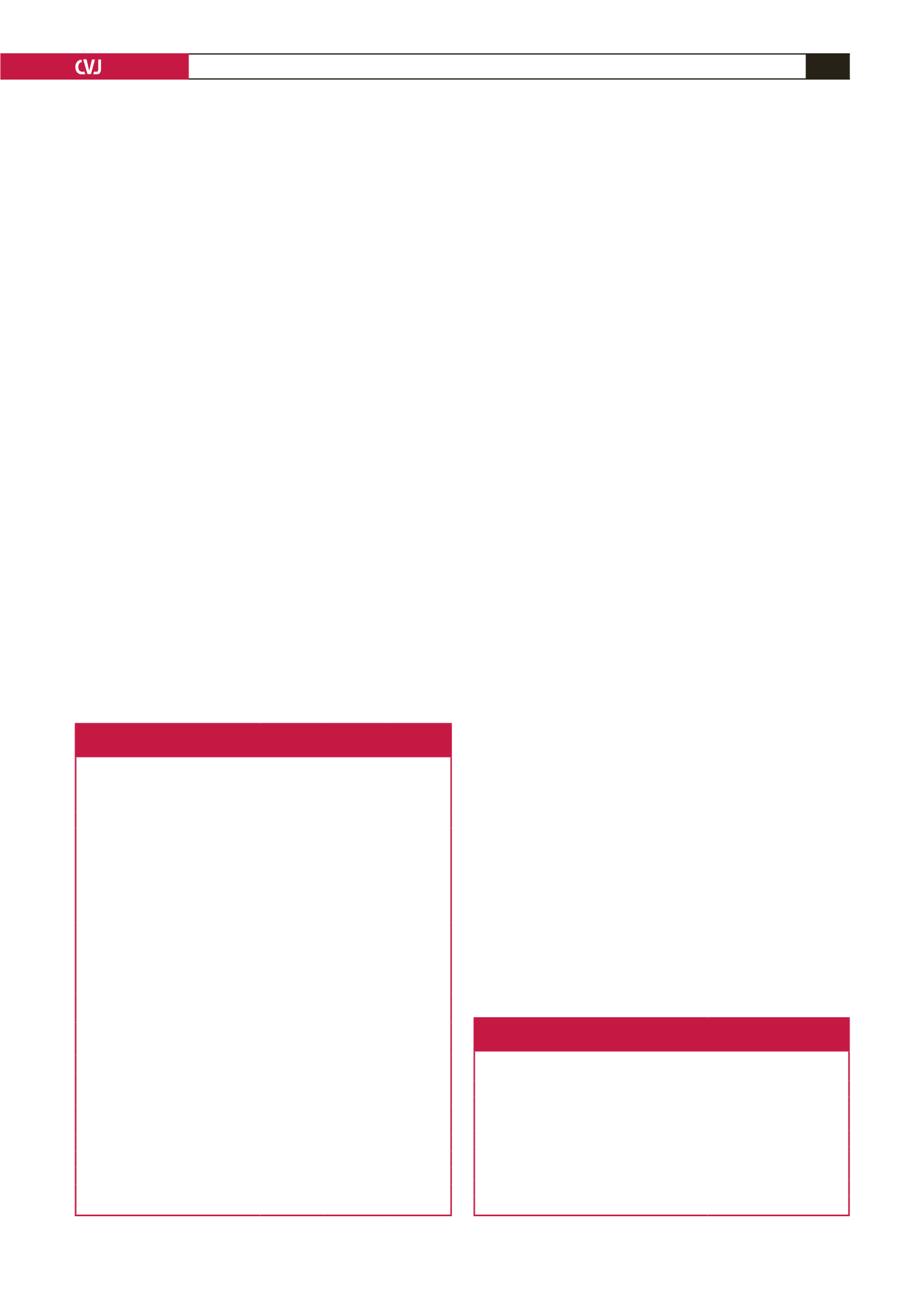
Table 2. Baseline characteristics and medical history for ODYSSEY
OLE participants in South Africa
Variables
Placebo
in parent
study
(
n
=
62)
Alirocumab
in parent
study
(
n
=
105)
All
(
n
=
167)
Age (years), mean (SD)
55.4 (10.7) 55.6 (12.6) 55.5 (11.9)
Gender (%, male)
45.2
39.0
41.3
Race (%)
White
Asian
Other
Black
White/Asian
85.5
1.6
0
9.7
3.2
87.6
0
3.8
4.8
3.8
86.8
0.6
2.4
6.6
3.6
Body mass index (kg/m
2
), mean (SD) 29.97 (6.09) 30.90 (6.40) 30.55 (6.28)
Heterozygous familial
hypercholesterolaemia (%)
Confirmation by genotyping
WHO/Simon Broome criteria
22.6
77.4
18.1
81.9
19.8
80.2
Atherosclerotic cardiovascular
disease (%)
56.5
42.9
47.9
Coronary heart disease* (%)
54.8
41.9
46.7
Myocardial infarction (%)
24.2
21.0
22.2
Unstable angina (%)
16.1
9.5
12.0
Ischaemic stroke (%)
8.1
3.8
5.4
Peripheral arterial disease (%)
3.2
1.9
2.4
Coronary revascularisation
procedures (%)
32.3
26.7
28.7
Hypertension (%)
58.1
47.6
51.5
Type 1 or 2 diabetes mellitus (%)
19.4
10.5
13.8
Family history of premature CHD 58.1
57.1
57.5
*According to information gathered and adverse events recorded during the
parent study as well as during the pre-treatment period of the OLE study.
Table 3. Background lipid-modifying therapy at baseline of the
ODYSSEY OLE study
Lipid-modifying therapy
All,
n
(%)
(
n
=
167)
High-intensity statin
108 (64.7)
Atorvastatin (40 or 80 mg)
61 (36.5)
Rosuvastatin (20 or 40 mg)
45 (26.9)
Simvastatin (40 or 80 mg)
37 (22.1)
Ezetimibe
46 (27.5)
Nutraceuticals
4 (2.4)
Change in statin therapy after enrolment in OLE
42 (25.1)
Used in combination with statins or not. May include ezetimibe.



















