
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 5, September/October 2019
AFRICA
287
Comparison between the groups in terms of the culprit vessel
affected andmultivessel frequency showed no significant differences.
The incidence of MACE and major and minor bleeding
during the hospital stay and at follow up are shown in Table
3. Only one patient developed major bleeding due to upper
gastrointestinal bleeding. Five patients developed minor bleeding
in group A (three patients developed access-site bleeding and two
developed haematuria). In group B, one patient developed major
bleeding in the lower gastrointestinal system and four developed
haematuria.
Discussion
Diabetic patients usually have microangiopathy and
microvascular dysfunction. After restoration of normal blood
flow in the coronary arteries, there is still insufficient myocardial
tissue reperfusion (i.e. no reflow and slow flow) in up to 30%
of patients.
19,20
Higher incidence of re-infarction, heart failure,
stroke and death was previously documented in diabetic than in
non-diabetic patients.
21
The main cause of slow flow and no reflow is thrombosis and
microvascular embolisation. These microvascular complications
are higher in AMI and primary PCI. Visible thrombus in
coronary angiography can be removed by a suction catheter, but
it was found that 61% of the thrombus was invisible in AMI.
22
Imperfect inhibition of platelet aggregation during PCI may
increase the MACE. The use of adjuvant medical drugs such as
GPIs considerably decrease the incidence of distal embolisation
and thrombotic outcomes in STEMI patients.
23,24
This study demonstrated that IC tirofiban administered for
thrombotic complications or bail-out situations, in addition to
loading oral antiplatelets in diabetic patients, was associated
with greater reduction of peak hs-TnT, CK-MB levels and
ST-segment resolution compared with IV tirofiban. Both
regimens showed similar results for MACE and major and minor
bleeding events during hospitalisation and after one month of
follow up. The risk of bleeding did not appear to increase with
Table 1. Baseline characteristics of both groups
Parameters
Group A (IV)
(
n
=
50)
Group B (IC)
(
n
=
45)
t/
χ
2
p-
value
Age (mean
±
SD)
58.56
±
10.18 55.90
±
11.66 0.72 0.41
Gender,
n
(%)
Male
27 (54)
23 (51.1) 0.69 0.49
Female
23 (46)
22 (48.9)
Body mass index
(kg/m
2
)
(mean + SD)
26.1
±
6.5
25.4
±
8.2 0.1
0.78
Smoking,
n
(%)
34 (68)
31 (68.8) 0.69 0.48
Hypertension,
n
(%)
20 (40)
19 (42)
0.08 0.78
Family history of coronary
artery disease,
n
(%)
9 (18)
7 (15.5) 0.61 0.54
Killip class > 1,
n
(%)
9 (18)
11 (24)
1.025 0.33
Aspirin,
n
(%)
49 (98)
43 (95.5) 0.05 0.87
Clopidogrel,
n
(%)
50 (100)
44 (97.7) 0.84 0.64
Beta-blockers,
n
(%)
41 (82)
39 (86.6) 0.06 0.85
ACEI or ARBs,
n
(%)
39 (78)
36 (80)
0.12 0.79
Statin,
n
(%)
44 (88)
39 (86.6) 0.15 0.73
Warfarin,
n
(%)
3 (6)
1 (2.2)
0.8
0.068
Onset-to-balloon time (min)
(mean
±
SD)
167
±
12.4
151
±
18.3 5.8
0.089
Door-to-balloon time (min)
(mean
±
SD)
46.8
±
8.9
44
±
7.6 1.72 0.38
Fasting glucose (mg/dl)
(mean
±
SD)
168
±
29.8
192
±
46.6 3.64 0.074
Glycated haemoglobin
(HbA
1c
) (mean
±
SD)
7.8
±
2.2
9
±
1.3 3.1
0.087
Creatinine (mg/dl)
(mean
±
SD)
1.17
±
0.41 1.08
±
0.56 2.56 0.251
Low-density lipoprotein choles-
terol (mg/dl) (mean
±
SD)
132.6
±
46 147.09
±
51 2.79 0.091
ACEI: angiotensin converting enzyme inhibitor; ARB: angiotensin II receptor
blocker.
Group A
Group B
80
60
40
20
0
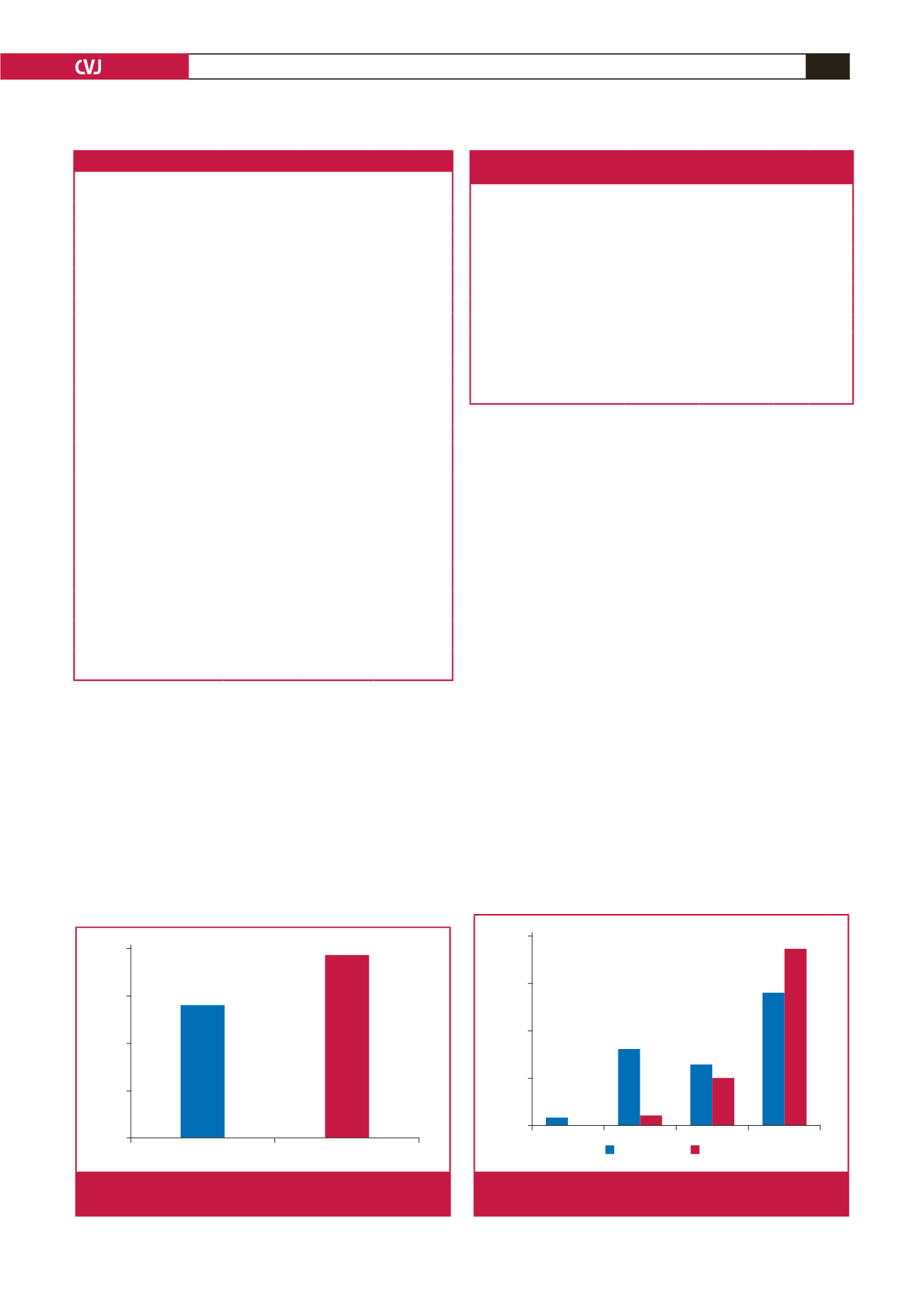
Fig. 1.
Frequency of 50% ST-segment resolution in the
groups.
Table 2. Comparison between the groups regarding cardiac
biomarkers and left ventricular ejection fraction
Parameters
Group A (IV)
(
n
=
50)
Group B (IC)
(
n
=
45)
t
p-
value
Peak CK-MB (U/l)
192.4
±
86 155.68
±
121 6.43 0.021*
Time to peak CK-MB (s)
12.9
±
5.8
8.96
±
3.2 11.4 0.001*
Peak hs-TnT (ng/dl)
#
5342
±
286 4291
±
334 5.9 0.035*
Time to peak hs-TnT (s)
13.5
±
3.1
9.24
±
2.8 10.7 0.001*
50% ST-segment resolution (%)
56
77
7.6 0.016*
LVEF at 48 hours (%)
38.6
±
5.3
41.5
±
3.2 0.84 0.632
LVEF at 30 days (%)
42.6
±
4.2
48.2
±
6.1 6.23 0.023*
Maximum C-reactive protein
level (ng/dl)
9.2
±
2.3
5.7
±
1.4 6.1 0.026*
#
Normal high-sensitivity troponin level up to 14 ng/dl.
CK-MB: creatine kinase-muscle/brain; hs-TnT: high-sensitivity troponin T;
LVEF: left ventricular ejection fraction.
0
I
II
III
100
75
50
25
0
Group A
Group B
Fig. 2.
Comparison of TIMI flow post intervention in the
groups.



















