
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 6, November/December 2019
318
AFRICA
anticoagulant in 55 (75.3%) of the patients and 18 (24.7%) were
on combined warfarin and aspirin anticoagulation.
Only 30 (41.1%) patients reported perfect adherence to their
medication, while the rest reported that they had missed a few
to several doses in the preceding six months. The most common
reason for missed doses was forgetfulness, accounting for about
22 (30.1%) of the cases, as reported by the patients themselves.
The next most common one was shortage or unavailability of
warfarin, accounting for 17 (23.3%) of the cases. Self-perceived
side effects and other various reasons accounted for the rest.
Forty-nine (67.1%) patients reported that they had scheduled
monthly visits with clinicians, while seven (9.6%) reported
that they visited less than once in three months. Thirty-three
(45.2%) of the patients reported that they hardly complied with
frequency of INR checks as prescribed by their doctors, and the
major reason given was cost and availability of the test. Table 2
shows responses and findings in patients with prosthetic heart
valves on anticoagulant treatment.
Educational level of primary school or less, more than 300
km distance from follow-up medical facility, quarterly or less-
frequent check-up visits, and source of free warfarin supply
being from a public institution were found to be significantly
associated with sub-optimal control of INR (Table 3). Multiple
other factors, including young age, parental level of education,
combination of warfarin and aspirin, missed anticoagulant
doses and lack of dietary counselling showed a tendency towards
an association but did not reach statistically significant levels.
A total of seven patients had major bleeding or stroke in
the course of their treatment and four of these patients died
as a result (Table 4). One of the fatalities had two episodes of
stroke, for which she was admitted. This patient died on the
third admission as a result of intracranial bleeding (patient #7).
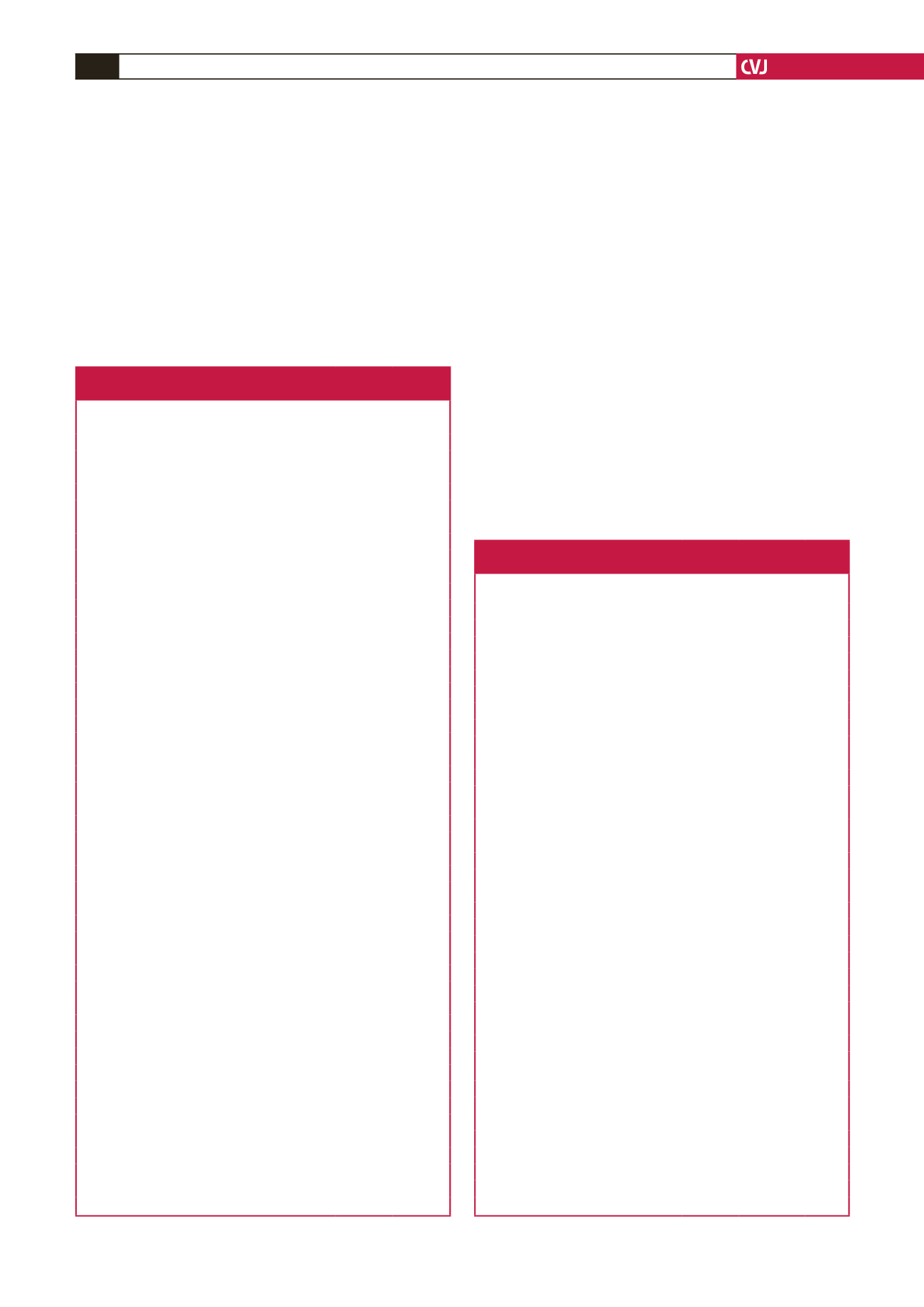
Table 2. Socio-demographic and clinical characteristics of patients
with prosthetic heart valves taking anticoagulants
Characteristics
Frequency Percentage
Age at the time of study (years)
11–15
6
8.7
16–20
16
23.2
21–25
47
68.1
NYHA functional class (at the time of study)
I
61
88.4
II
7
10.1
III
1
1.5
IV
–
–
Prosthetic valve position
Mitral
49
67.1
Aortic
9
12.3
Mitral and aortic
14
19.2
Other
1
1.4
INR control
Optimal
35
47.9
Sub-optimal
38
52.1
Educational status of the patient
≤ Primary education
25
34.3
Secondary education
29
39.7
Higher education
19
26.0
Parental education (best)
≤ Primary education
34
46.6
Secondary education
13
17.8
Higher education
26
35.6
Distance from cardiology care clinic (km)
≤ 150
55
75.3
151–300
4
5.5
> 300
14
19.2
Anticoagulant
Warfarin alone
55
75.3
Warfarin + aspirin
18
24.7
Drug supply source
Private
19
26.0
Public for payment
36
49.3
Public for free
18
24.7
Frequency of INR determination
Every month
54
74.0
Every 2 months
4
5.5
Quarterly or longer
15
20.5
Laboratory facility for INR
Private
73
100
Public
–
–
Missed doses (approximate)
Never
30
41.1
1–2 doses per week
34
46.6
> 2 doses per week
9
12.3
Bleeding or thromboembolic complications
7
9.6
Table 3. Factors associated with sub-optimal control of INR
in patients with prosthetic heart valves
Factors analysed for association
Optimal
control
Sub-optimal
control
p
-value
Age at surgery (years)
<
15
7
10
0.588
≥ 15
28
28
Gender
Female
21
21
0.813
Male
14
17
Educational status of the patients
≤ Primary education
6
19
0.003
≥ Secondary education
29
19
Parental/caretaker education (best)
≤ Primary education
14
20
0.350
≥ Secondary education
21
18
Distance from follow-up facility (km)
<
300
32
23
0.003
≥ 300
3
15
Clinic visit frequency
Once in a month
28
21
0.022
Once in a quarterly or less
7
17
Approximate monthly income ($US)
≤ 50
14
12
0.162
> 50
21
16
Medications
Warfarin alone
28
27
0.425
Warfarin + aspirin
7
11
Source of medication supply
Private or public for fee
30
25
0.047
Public for free
5
13
Medication adherence counselling
(as per patient’s report)
Yes
32
33
0.712
No
3
5
Dietary counselling (as per patient’s report)
Yes
24
20
0.232
No
11
18
Anticoagulant doses missed (approximate)
None or
<
1 dose per week
33
31
0.155
≥ 1 dose per week
2
7



















