
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 6, November/December 2019
AFRICA
325
prevalence of diabetes (30.4 and 26.7%) and screen-detected
diabetes (8.7 and 9.2%) was similar in men and women,
respectively (
p
=
0.249).
Post-menopausal women had higher systolic blood pressure
(SBP), fasting glucose (
p
<
0.001), two-hour glucose (
p
=
0.01),
triglyceride (
p
<
0.01), TC (
p
<
0.05) and HDL-C (
p
<
0.001)
concentrations than pre-menopausal women. The prevalence
of impaired glucose tolerance (IGT)/impaired fasting glucose
(IFG) and type 2 diabetes was similar in the pre-and post-
menopausal women (
p
=
0.166).
Table 3 shows the associations between body fat variables and
cardiometabolic risk factors in the whole sample, adjusting for
gender and age. In terms of total body fat (kg and %), positive
associations were observed for diastolic blood pressure (DBP) (
p
<
0.05), two-hour glucose, fasting insulin, HOMA-IR (all
p
<
0.01)
and triglyceride concentrations (
p
<
0.05) as well as hsCRP, and in
the case of body fat %, TC (
p
<
0.01) and LDL-C levels (
p
<
0.05).
When examining associations between central fat mass
(trunk fat %FM, android %FM, VAT and SAT area) and
cardiometabolic risk profile, we found positive associations with
DBP, fasting glucose, two-hour glucose, fasting insulin, HOMA-
IR, triglyceride and hsCRP concentrations (
p
<
0.01 for all), and
negative association with HDL-C levels (
p
<
0.01 for all). When
examining the relationships of peripheral fat mass, we found that
arm fat mass was positively associated with SBP (
p
<
0.05), DBP
(
p
<
0.01), levels of fasting insulin (
p
<
0.05) and HOMA-IR (
p
<
0.01), and negatively associated with HDL-C (
p
<
0.01) levels.
By contrast, lower body peripheral fat mass (gynoid %FM and
leg %FM) was negatively associated with all CVD risk markers,
except for HDL-C, which was positively associated with gynoid
and leg %FM (
p
<
0.01).
We then compared the proportion of the variance that
age, gender and the different body composition measures
explained for each cardiometabolic risk factor. Together with
age and gender, VAT area accounted for the greatest variance
in fasting insulin (29%) and HOMA-IR (27%) levels, while
SAT area accounted for the greatest variance in hs-CRP (15%)
concentrations. Trunk %FM and leg %FM contributed equally
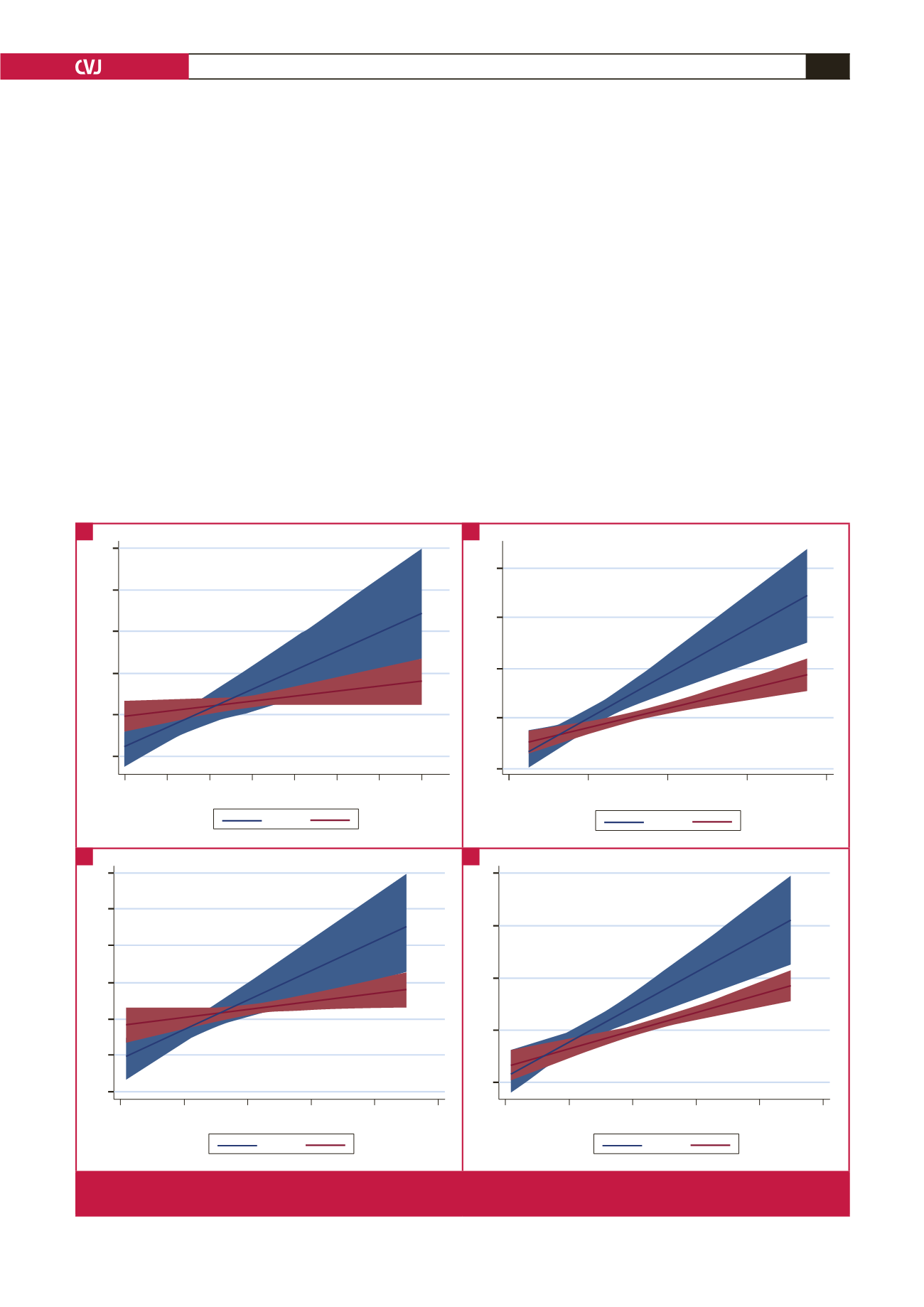
Men:
r
= 0.702,
p
≤
0.001
Women:
r
= 0.205,
p
≤
0.007
2 hr glucose (mmol/l)
14
12
10
8
6
4
5 15 25 35 45 55 65 75
Body fat (kg)
M F
Men:
r
= 0.780,
p
≤
0.001
Women:
r
= 0.424,
p
≤
0.001
HOMA-IR
8
6
4
2
0
0 20 40 60 80
Body fat (kg)
M F
Men:
r
= 0.720,
p
≤
0.001
Women:
r
= 0.204,
p
≤
0.008
2 hr glucose (mmol/l)
14
12
10
8
6
4
2
0 200 400 600 800 1000
SAT (cm
2
)
M F
Men:
r
= 0.745,
p
≤
0.001
Women:
r
= 0.440,
p
≤
0.001
HOMA-IR
8
6
4
2
0
0 200 400 600 800 1000
SAT (cm
2
)
M F
Fig. 1.
Gender-specific associations between total body fat and abdominal subcutaneous adipose tissue (SAT) and two-hour
glucose (A, C) and insulin resistance, estimated using HOMA-IR (B, D), respectively.
A
C
B
D



















