
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 2, March/April 2020
66
AFRICA
hour, grade 2:
>
30 extrasystoles per hour, grade 3: multiform
ventricular extrasystoles, grade 4a: two consecutive ventricular
extrasystoles, and grade 4b: three or more consecutive ventricular
extrasystoles.
Shortly before discharge from hospital, a technetium (
99m
Tc)
methoxyisobutylisonitrile (sestaMIBI) test was performed using
a two-day protocol in which
99m
Tc sestaMIBI was administered
at rest (day 1) and at peak stress (day 2). Exercise stress and/or
coronary vasodilator pharmacological stress using dipyridamole
was used. Atropine was given at peak stress if the heart rate
was less than 120 beats per minute. Imaging was performed
using a Siemens e.cam (Munich, Germany) one-hour post
injection. Attenuation correction was done in all overweight
patients. SestaMIBI processing was done using 4DM SPECT
software. Analysis was done using Siemens Axiom Artis software
(Munich, Germany).
99m
Tc sestaMIBI findings were reported as normal, areas of
infarction, or ischaemia. A scan was defined as normal when
there was complete uptake of the radioisotope at rest, with no
change post stress. Ischaemia was defined as an area of absent
or reduced uptake on stress that shows normalisation during rest
(i.e. reversibility). An infarct was defined as an area of absent
or reduced uptake on stress that remained fixed at rest (i.e. no
reversibility).
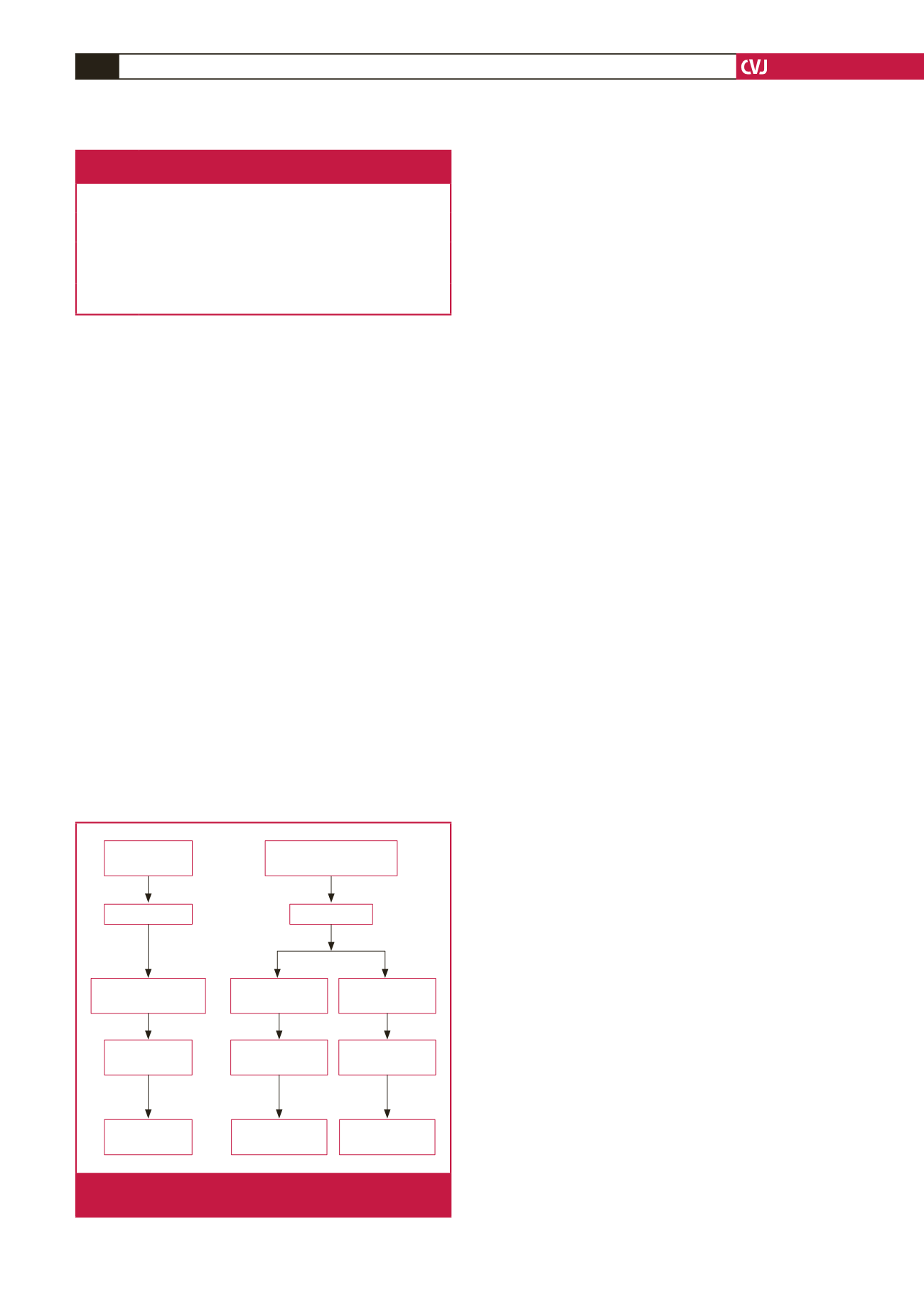
Two groups of subjects were included in the study to assess
the effects of acid installation independent of concomitant
ischaemia. Patients referred to the gastrointestinal unit at
Addington Hospital with heartburn, who were diagnosed with
erosive reflux oesophagitis at EGD, comprised the GORD group
(Fig. 1). Subjects in whom the endoscopy was normal were also
selected as normal control subjects. All subjects underwent acid
instillation and Holter recording.
Informed consent was obtained from all individuals in the
study and approval was granted by the bio-ethics committee of
the Faculty of Health Sciences, Nelson R Mandela School of
Medicine, University of KwaZulu-Natal.
Statistical analysis
Data analysis was conducted using SPSS (Statistical Packages
for the Social Sciences) software (version 23). A
p
-value
<
0.05
was deemed as statistically significant. A descriptive statistical
analysis of the data (means and percentages) was initially
conducted prior to inferential analysis. Proportions were used
to estimate the prevalence of GORD in subjects with ACS.
Difference in the proportions of ischaemia/infarction between
study and control groups was analysed using the Pearson
chi-squared test as well as determining whether the presence of
GORD could trigger ischaemic events. Logistic regression was
used to assess the odds of developing ST changes after acid
instillation. Means for the groups were compared using one-way
analysis of variance, followed by the Tukey
post hoc
test.
Results
A total of 376 patients underwent consecutive endoscopy. The
111 subjects with ACS were admitted to the CCU. They were
stable and underwent endoscopy to determine the presence of
oesophagitis (Fig. 1). Of these ACS subjects, 39 had grade A
reflux oesophagitis and constituted the ACS study group.
Of the 265 patients with dyspepsia, 27 had GORD with
grade A reflux oesophagitis. Seven of these subjects had either
reversible (ischaemic) or fixed (infarct) changes on the sestaMIBI
scan and were excluded, leaving 20 subjects with isolated GORD.
None of the controls showed any reversible (ischaemic) or fixed
(infarct) changes on the sestaMIBI scan, indicating they were
also free of significant coronary artery disease.
There were 30 males and nine females (mean age 52 and 51
years, respectively) in the ACS group. These 39 subjects comprised
35 (89.7%) with ST-elevation myocardial infarction (MI) (45.7%
were in the inferior territory, 25.7% anterior and 28.6% lateral)
and four (10.3%) subjects with non-ST-elevation MI.
There was no significant difference in the age distribution
between ACS subjects and those with isolated GORD. There
was no difference in body mass index between the controls and
ACS subjects (
p
=
0.974) but waist measurements were lower in
the control subjects (ACS vs control
p
=
0.003; GORD vs control
p
=
0.002) (Table 2).
As expected, risk-factor analysis revealed that incidence of
diabetes mellitus, hypertension and smoking were more frequent
in the ACS group. Control subjects were free of hypertension,
hypercholesterolaemia and diabetes. Plasma glucose level was
elevated in male subjects in both the ACS and GORD groups,
but was normal in the controls (
p
<
0.001). Risk-factor clustering
in the form of the metabolic syndrome was present in 17/39
(44%) in the ACS group, 1/20 (5%) in the GORD group and
none in the control group.
Control subjects
(screened 265 subjects)
ACS (111)
Endoscopy
Endoscopy
ACS + erosive GORD
(39)
Erosive GORD
(27)
Normal (22)
MIBI
7 abnormal MIBI
subjects excluded
Normal MIBI
ACS (39)
Erosive GORD
(20)
Controls (22)
Fig. 1.
Selection of subjects for the study. All subjects under-
went endoscopy and sestaMIBI scanning.
Table 1.The Los Angeles classification of oesophagitis
(Armstrong
et al
. Gastroenterology 1996).
Grade A One (or more) mucosal break no longer than 5 mm that does not
extend between the tops of two mucosal folds
Grade B One (or more) mucosal break more than 5 mm long that does not
extend between the tops of two mucosal folds
Grade C One (or more) mucosal break that is continuous between the tops
of two or more mucosal folds but which involves less than 75% of
the oesophageal circumference
Grade D One (or more) mucosal break that involves at least 75% of the
oesophageal circumference



















