
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 3, May/June 2020
AFRICA
137
Methods
A prospective cohort study was conducted from 2010 to 2016
at a tertiary multidisciplinary maternal care facility in Cape
Town, South Africa.
This is an analysis of an ongoing cohort
for which data on methodology, overall patient characteristics
and diagnosis, as well as six- and 12-month outcome has been
published recently.
29,30
All patients gave written informed consent. All principles
from the Declaration of Helsinki were adhered to. The study
was approved by the ethics committee of the University of Cape
Town (HEC ref: 173/2010).
Of 178 consecutive pregnant womenwith SHD, 24.2%received
BBs (
n
=
43) in pregnancy. Data were manually extracted from
both cardiology and obstetric clinical records, after screening for
eligibility, and captured in a modified database. Data parameters
recorded included gestational age, gender, mode of delivery,
birth weight and Apgar scores for all patients. Data on type of
BB used, treatment dosage, treatment duration in weeks and
trimester of BB initiation were additionally recorded for the BB
group. The type of BB available and prescribed in South African
public service hospitals was recorded. Atenolol and carvedilol
are the only BBs approved for provincial service in South Africa.
SHD pregnancies were sub-divided into congenital, valvular,
cardiomyopathy and ‘other’ for extended analysis. The subgroup
‘other’ included infiltrative heart disease such as sarcoidosis,
ischaemic heart disease and heart disease caused by arrhythmias.
Patient exclusion criteria included: (1) essential information
regarding birth weight, and gestational age not available, (2)
pregnancies not exceeding 24 weeks of gestation, and (3)
therapeutic abortions at any gestational period. Adverse foetal
outcomes were defined as: perinatal death, LBW defined as
birth weight
<
2 500 g, Apgar scores
<
7 and premature birth
(
<
37 weeks).
Statistical analysis
The descriptive statistics are stated as frequency, median and
interquartile range or mean value and standard deviations where
applicable. Comparison of continuous variables between case
and control groups was performed using unpaired Student’s
t
-tests for data normally distributed. Otherwise the Mann–
Whitney
U
-test was used. To compare categorical variables, the
chi-squared or two-tailed Fisher’s exact test was used where
appropriate;
p
<
0.05 was considered to be significant at the 95%
confidence level.
Finally, we correlated the treatment duration of oral BBs with
the relative deviation from expected FBW for the 24 patients for
whom data were available. Data analysis was performed using
SPSS 24 for Windows. Figures were created with GraphPad
Prism 7 for Windows, Version 7.03.
Results
Baseline characteristics of all pregnancies are shown in Table
1. Pregnant women exposed to BBs were older than those
who were not. No significant differences were noted between
the groups for clinical and echocardiographic parameters.
When dividing pregnancies into those with New York Heart
Association (NYHA) I–II and III–IV physical limitation, a
significant increase (
p
=
0.001) was noted between the number
of pregnancies exposed to BBs compared to those not exposed.
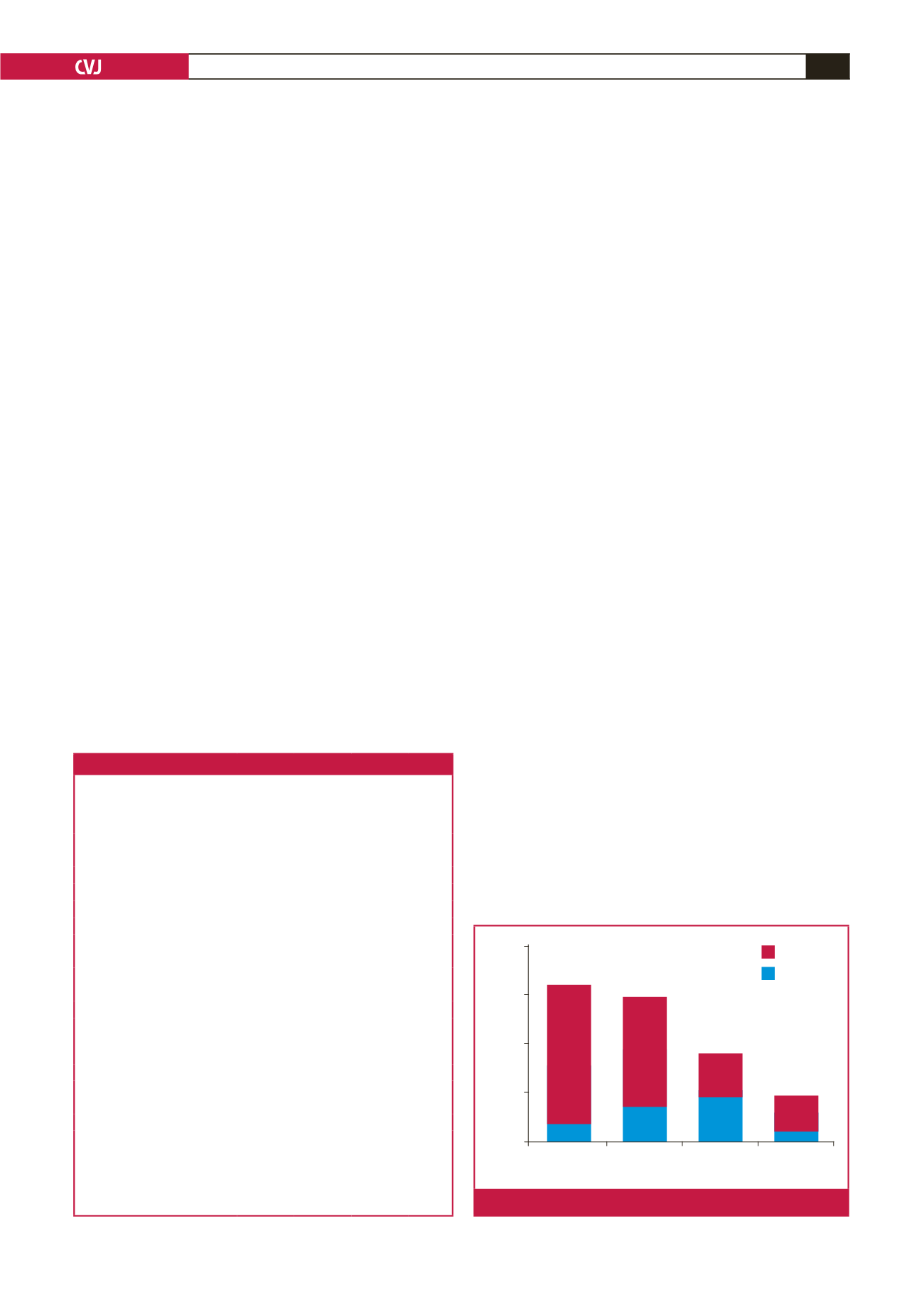
Of the 178 patients analysed in this study, 64 (36%) presented
with CHD, indicating predominance within this subgroup
compared to valvular heart disease (33.1%), cardiomyopathy
(20.2%) and ‘other’ (10.7%) (Fig. 1). Dividing BB use among
the four subgroups revealed higher BB usage within the valvular
(32.6%) and cardiomyopathy (41.9%) subgroups.
BB exposure during pregnancy was found to be associated
with a non-significant increased mean FBW (2 912 vs 2 807 g,
p
=
0.347) and a similar mean gestational age of delivery (GAD)
(37.4 vs 37.5 weeks,
p
=
0.841) (Fig. 2A, B). The outcomes of
mean GAD in weeks and mean FBW among the four subgroups
are shown in Table 2. The highest mean GAD and FBW were
found in the valvular (37.7 weeks) and cardiomyopathy (2 999 g)
subgroups, respectively. Lowest mean FBW was in the ‘other’
group and lowest mean GAD occurred in the cardiomyopathy
group. When comparing the different types of BBs used (atenolol
Table 1. Baseline maternal characteristics of study population (
n
=
178)
Clinical characteristic
All
(
n
=
178)
BB used
(
n
=
43)
BB not
used
(
n
=
135)
p
-value
Age (years)
28
±
6
30
±
6
28
±
6 0.008
Parity,
n
(range)
2 (1–5)
2 (1–4)
1 (1–5)
0.153
BMI (kg/cm
2
)
28.1
±
7.3 28.4
±
7.0 27.9
±
7.4 0.664
Systolic blood pressure (mmHg)
121
±
16 121
±
17 121
±
15 0.721
Diastolic blood pressure (mmHg) 74
±
12 76
±
13 73
±
12 0.199
Heart rate (beats/min)
86
±
17 88
±
15 85
±
12 0.176
NYHA functional class,
n
(%)
I/II
152 (88)
31 (74)
121 (92)
0.001
III/IV
21 (12)
11 (26)
10 (8)
Haemoglobin (g/dl)
11.6
±
1.7 11.7
±
1.5 11.5
±
1.7 0.340
Echocardiography
LVEDD (mm)
48.5
±
7.6 50.1
±
8.3 48.1
±
7.3 0.112
LVESD (mm)
33.6
±
7.6 35.5
±
9.7 33.0
±
6.7 0.099
Ejection fraction (%)
58.6
±
11.8
56.1
±
13.7
59.6
±
10.5
0.132
General medical history (%)
Chronic hypertension
17 (10)
4 (9)
13 (10)
0.949
HIV
38 (21)
9 (21)
29 (21)
0.921
Family history of CVD
31 (17)
7 (16)
24 (17)
0.843
Caesarian section,
n
(%)
90 (51)
25 (58)
65 (48)
0.291
Values are mean
±
SD unless otherwise specified.
p
-values based on unpaired
t
-tests, Mann–Whitney
U
-tests or chi-squared tests where appropriate.
BB, beta-blockers; BMI, body mass index; CVD, cardiovascular disease; LVEDD,
left ventricular end-diastolic diameter; LVESD, left ventricular end-systolic diam-
eter; NYHA, New York Heart Association; HIV, human immunodeficiency virus.
Congenital
Valvular
Cardio-
myopathy
Other
Number of patients
80
60
40
20
0
BB not used
BB used
Fig. 1.
Distribution of BB groups among the SHD subgroups.



















