
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 4, July/August 2020
192
AFRICA
had coronary heart disease, one had no dilated cardiomyopathy
and two others had no cardiac abnormalities. Three patients
were lost to follow up. We confirmed the vital status of 243
patients through medical files and by phone; three patients had
been transferred to other provinces.
Therefore, of the 240 confirmed alive and who had not
moved, echocardiography was performed on 196 patients
(121 with normal hearts and 75 who had abnormalities at
baseline); it could not be done on the remaining 44 (14.2%).
The echocardiographic features were unchanged in 165 (84.2%)
patients. Progression with no clinical relevance occurred for
minor mitral valve abnormalities (17/33, 51.5%) and LV systolic
dysfunction (10/29, 34.5%), not meeting criteria for either RHD
or cardiomyopathy. Two patients with RHD had been treated,
and two patients with abnormal LV ejection fraction recovered
their systolic function.
At the five-year follow up, 18 patients of the 243 alive at the
24-month follow up had died (Fig. 1). Of these, 10 had cardiac
abnormalities at baseline: abnormal relaxation (three) and
thickened mitral valve (three), while the rest had RHD aortic
regurgitation, moderated pulmonary arterial hypertension, left
ventricular hypertrophy and reduced systolic function. Five
patients had abandoned the treatment and were lost to follow up.
Overall, 24 (9.5%) out of the 252 patients had died at five years
and eight (3.2%) had been lost to follow up.
Discussion
This study of young HIV-infected African individuals on
chronic ART revealed a latent cardiovascular risk, as assessed
by overweight, obesity, anaemia and systemic hypertension.
Additionally, more than one-third of the patients had
echocardiographic abnormalities; the most important being
rheumatic heart valve disease, impaired LVSF and diastolic
dysfunction, but the disease was clinically relevant in only a few
patients. None of these patients had been investigated or treated
for these conditions.
Our cohort had lower occurrence of clinically significant
dilated cardiomyopathy and pericardial effusion, in contrast
with cohorts from similar settings in Africa described before
the advent of ART.
10,11
For instance, years ago in South Africa,
the most common cardiovascular HIV-related presentations
were cardiomyopathy (38%), pericardial disease (13%) and
pulmonary arterial hypertension (8%).
12
Similarly, a study of
102 HIV-infected patients in Tanzania, of whom 54.7% were
in WHO HIV clinical stage III–IV, reported large symptomatic
pericardial effusions in 5.9%, dilated cardiomyopathy in 9.8%
and pulmonary arterial hypertension in 12.7%.
13
Indeed, before the advent of ART, cardiotropic virus infection
and myocarditis were considered the most critical factors
involved in the pathogenesis of symptomatic HIV-associated
cardiomyopathy,
14,15
but recent data from Africa show marked
reduction in the prevalence of HIV-related cardiac disease with
the use of ART.
16,17
However, our results reveal high occurrence of
asymptomatic systolic dysfunction that needs to be highlighted
to promote its early detection and improve prognosis, namely
with the use of beta-blockers, vasodilators and anti-arrhythmia
drugs.
18
Our findings corroborate the concept that urban African
settings that are epicentres of the HIV epidemic also have
rising levels of lifestyle factors characteristic of epidemiological
transition, being at the crossroads between prevalent diseases
caused by infections such as tuberculous pericarditis, RHD,
HIV, and cardiovascular diseases such as arterial hypertension
and coronary artery disease. Increased access to ART, due to its
effects on lipid and glucose metabolism,
19,20
is expected to result
in higher numbers of people at risk of cardiovascular disease.
In this context, cardiovascular risk assessment of HIV-infected
patients in Africa will become a critical element of care, similar
to what is recommended for developed settings. Therefore, to
ensure tailored and comprehensive patient care in underserved
areas, algorithms using risk prediction and clinical evaluation
rules for endemic conditions should be developed, to be used by
non-specialists.
The ART effects contributing to change in cardiovascular
disease profile in endemic areas for HIV in Africa may be more
pronounced as countries adhere to the 90-90-90 strategy.
21
Increase in blood pressure after 48 weeks of ART occurred
during a prospective observational study of 95 HIV-positive
patients in Spain, dependent on age and high BMI.
22
However, a
longitudinal analysis of 17 170 patients who were submitted to 73
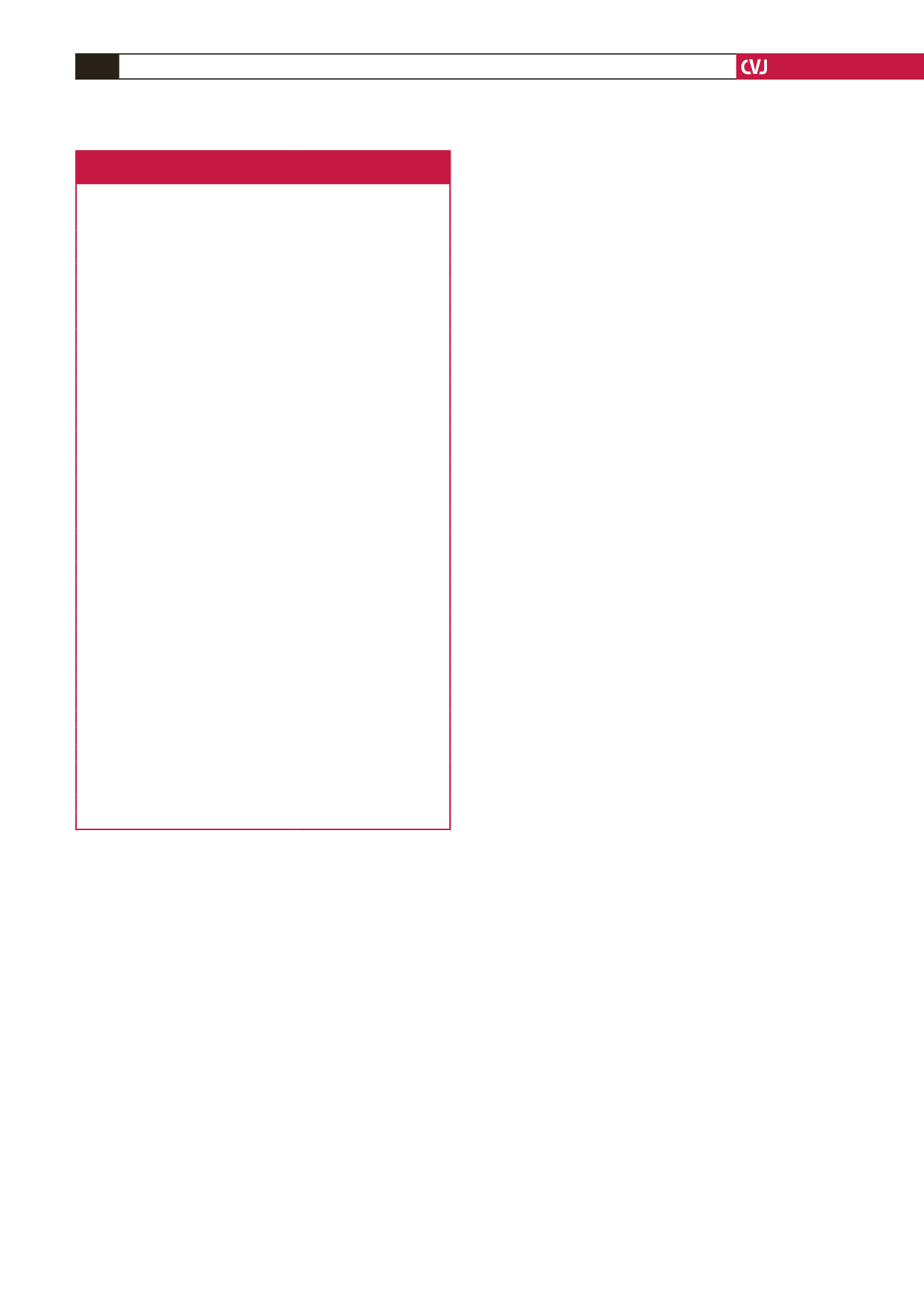
Table 1. Demographic, clinical, laboratory and echocardiographic
data of the 264 HIV-infected patients
Variables
Frequency (%) or mean ± SD
(
n
= 264)
Age, years
39.3 ± 9.8
18–25,
n
(%)
10 (3.8)
26–45,
n
(%)
188 (71.2)
46–65,
n
(%)
64 (24.2)
≥ 65,
n
(%)
2 (0.8)
BMI,
n
(%)
Obesity > 30 kg/m
2
45 (17.0)
Overweight
65 (24.5)
Underweight
11 (4.2)
High BP,
n
(%)
54 (20.5)
ART
Time of ART exposure (months)
46 (± 36)
Therapy with DUOVIR-N
192 (± 72.7)
WHO clinical stage,
n
(%)
I
173 (65.5)
II
40 (15.2)
III
45 (17.0)
IV
6 (2.3)
Laboratory examinations
CD4 cell counts
516 ± 641
Viral load < 50 copies/ml
174 ± 65.9
Glycaemia (mmol/l)
4.3 ± 1.5
Diabetes mellitus type 2,
n
(%)
4 (1.5)
Haemoglobin
11.9 ± 0.11
Anaemia
Female,
n
(%)
119/186 (64)
Male,
n
(%)
34/78 (44)
Echocardiographic findings (
n
= 252),
n
(%)
Rheumatic heart valve disease
6 (2.4)
Systolic dysfunction
29 (10.3)
Diastolic dysfunction
13 (5.2)
Aortic disease
3 (1.2)
Congenital heart disease
3 (1.2)
Pericardial effusion
2 (0.8)
Pulmonary arterial hypertension
2 (0.8)
Minor mitral valve abnormalities
33 (13.1)
Normal
164 (65.1)



















