CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 4, May 2013
112
AFRICA
(91%) (Table 3). Those presenting to TBH were more likely to
receive early
β
-blockade than were those presenting to the SH (67
vs 35%, respectively,
p
=
0.0055). This could not be accounted
for by a difference between WH and KBH where 41 and 31% of
patients received
β
-blockers, respectively (
p
=
0.4839).
While the clinical presentation and initial medical management
was largely similar for the two cohorts, there were significantly
more angiograms performed in the TBH group (94%) compared
to the SH group (51%) (
p
<
0.0001) (Table 4). Again this was
not due to differences in the frequency of invasive management
between WH (48%) and KBH (54%) in sub-analysis (
p
=
0.6633). There was also no difference in the frequency of
referral to TBH from WH or KBH (71 and 73%, respectively;
p
=
0.8588), and the acceptance rate of referrals was equally
high from both hospitals (92% for WH and 94% for KBH,
p
=
0.7347). Cases fromWH did however have a significantly longer
time to angiography than those from KBH (3
±
1.60 vs 1.5
±
1.22
days respectively,
p
=
0.0225).
At angiography, stenosis was seen in the left anterior
descending artery (LAD) in 72% of cases, in the right coronary
artery (RCA) in 72% and in the left circumflex (LCx) in 59%. In
80% of cases there was multi-vessel disease (40% double-vessel
and 40% triple-vessel disease); 6% had small-vessel disease.
If percutaneous intervention (PCI) was performed, the culprit
lesion was the RCA in 21%, the LCx in 21% and the LAD in
17% of cases.
When angiography was performed, both cohorts were equally
likely to receive coronary revascularisation via PCI (45% for
the SH and 68% for TBH,
p
=
0.1018). The SH group had more
TABLE 1. BASELINE CHARACTERISTICS
Secondary
hospitals
n
=
43
(%)
TBH
n
=
33
(%)
p
-value
Age (years) (
±
SD)
60.5 (
±
12.6) 61.0 (
±
14.88) 0.8774
Male
24 (56)
19 (58)
0.8779
Female
19 (44)
14 (42)
0.8779
Hypertension
33 (77)
23 (70)
0.4903
Diabetes mellitus
12 (28)
14 (42)
0.1868
Dyslipidaemia
16 (37)
20 (61)
0.0421*
Obesity
3 (7)
1 (3)
0.4319
Smoking
24 (56)
18 (52)
0.7993
Current
17 (40)
11 (33)
0.2641
Past
7 (16)
7 (21)
0.3873
COPD
3 (7)
2 (6)
0.8727
Ischaemic heart disease
16 (37)
17 (52)
0.2123
Stable angina pectoris
5 (12)
4 (12)
0.2123
Unstable angina pectoris
1 (2)
3 (9)
0.1905
Previous MI
10 (23)
9 (27)
0.6885
Previous angiography
9 (21)
10 (30)
0.3496
Previous stent
3 (7)
8 (18)
0.1340
Previous CABG
4 (9)
7 (21)
0.1436
Family history of IHD
4 (9)
5 (15)
0.4363
Prior asprin use within 7 days
20 (47)
23 (70)
0.0415*
Known stenosis
>
50%
7 (16)
11 (33)
COPD: chronic obstructive pulmonary disease, MI: myocardial infarction,
CABG: coronary artery bypass graft.
*
p
-values calculated comparing TBH and secondary hospital groups,
p
<
0.05 was statistically significant.
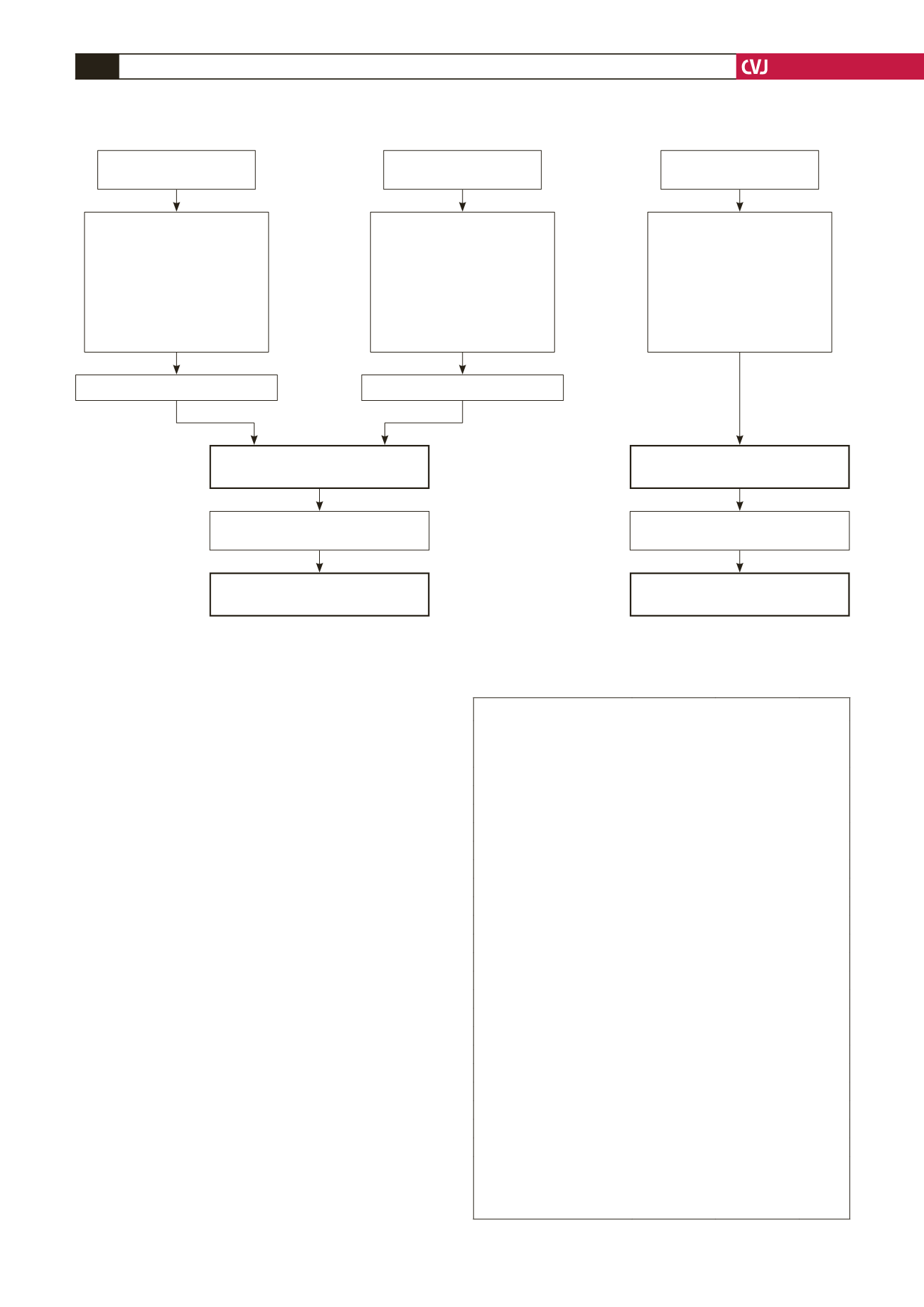
Fig. 1. Data capturing.
34 cases excluded:
• 18 STEMI
• 12 renal failure
• 3 anaemia
• 1 no folder available
56 cases excluded:
• 27 STEMI
• 13 renal failure
• 3 anaemia
• 3 sepsis
• 5 CVA
• 1 warfarin Rx
• 1 life expectancy
<
6 months
• 3 no folder available
WH = 17 NSTEMI cases included
Secondary hospitals = 43 NSTEMI
cases included at admission
• 10 died during index admission
• 3 lost to follow up
Secondary hospitals = 30 NSTEMI
cases included at 6 months
TBH = 33 NSTEMI cases included
at admission
• 2 died during index admission
• 3 lost to follow up
TBH = 28 NSTEMI cases included
at 6 months
KBH = 26 NSTEMI cases included
169 cases excluded:
• 63 referred from secondary
hospitals
• 79 STEMI
• 4 renal failure
• 6 anaemia
• 2 sepsis
• 2 warfarin Rx
• 13 no folder available
TBH = 202 cases
with positive troponin
KBH = 82 cases
with positive troponin
WH = 51 cases
with positive troponin
WH: Worcester Hospital, KBH: Karl Bremer Hospital, TBH: Tygerberg Hospital, NSTEMI: non-ST-elevation myocardial infarction, STEMI: ST-segment elevation
myocardial infarction, CVA: cerebrovascular accident.