CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 4, May 2013
AFRICA
113
stenosis of the left main stem (LMS) (
p
=
0.0477) and there was
a trend for cases from the SH to be more frequently referred for
coronary artery bypass grafting (CABG) (36 vs 26% in the TBH
cohort,
p
=
0.0795), the majority as in-patients.
Patients presenting to TBH directly had a better in-hospital
survival rate than those presenting to the SH (94 vs 77%,
p
=
0.0326) (Table 5). At six months there was a tendency to
better survival in the TBH group (90 vs 73%,
p
=
0.0614).
Most patients were discharged on aspirin,
β
-blockers, ACE
inhibitors and statins and remained pain free; 23% of cases were
re-admitted to hospital during follow up, most commonly with
unstable angina pectoris (UAP) (54%, data not shown); 16% of
cases underwent subsequent angiography.
As the numbers of patients re-admitted to hospital (nine for the
SH group and four for TBH) and those undergoing angiography
after discharge were small (six for the SH and three for the TBH
cohort), it was not possible to perform a meaningful statistical
analysis looking for differences between these groups; 66% of
these cases received coronary revascularisation, either via PCI
or subsequent CABG. Cases presenting to TBH underwent
subsequent angiography after 1.33
±
0.57 months, and those
from the SH after 4.5
±
2.07 months.
Discussion
The management of patients suffering an NSTEMI presenting to
the public health sector is affected by the level of service to which
the patient presents.This is not a result of geographical remoteness
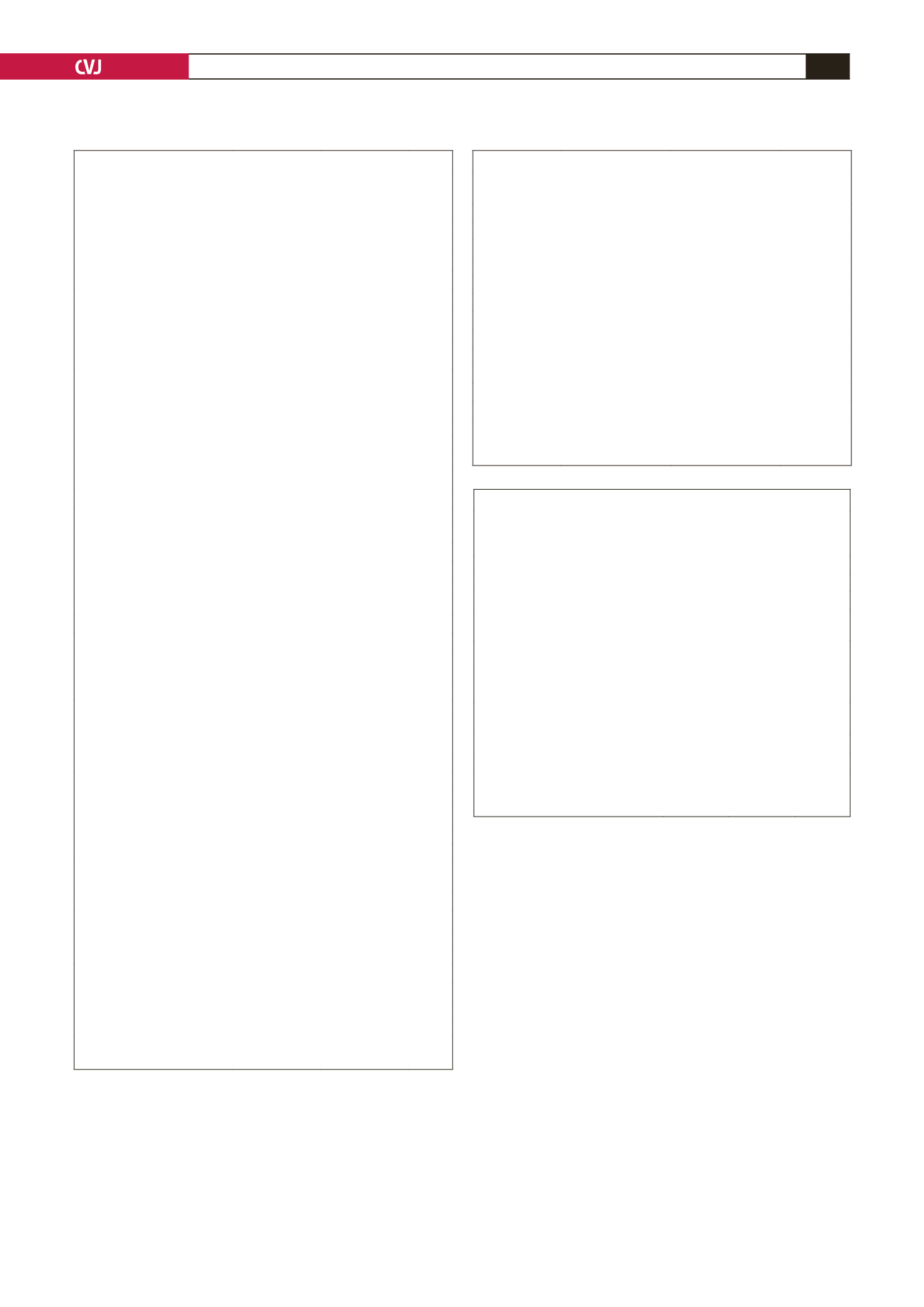
TABLE 4. INVASIVE MANAGEMENT ON INDEXADMISSION
Secondary
hospitals
n
=
43
(%)
TBH
n
=
33
(%)
p
-value
Angiography performed as in-patient
22 (51)
31 (94) < 0.0001*
Time (days from admission) (
±
SD)
2.14 (
±
1.52) 1.70 (± 1.65) 0.8615
Coronary revascularisation
Via PCI (expressed as a % of
angiography cases)
10 (45)
21 (68)
0.1018
Via PCI (expressed as a % of entire
group)
10 (23)
21 (64)
0.0004*
Via PCI or CABG (% of angiography
cases)
18 (82)
29 (94)
0.1842
Via PCI or CABG (expressed as a %
of entire group)
18 (42)
29 (88)
<0.0001*
No. of stents
1.3 (
±
0.48) 1.3 (± 0.91) 0.8952
Referred for CABG
8 (36)
8 (25)
0.0795
PCI: percutaneous coronary intervention, CABG: coronary artery bypass graft.
*
p
-values calculated comparing TBH and secondary hospital groups,
p
<
0.05 was statistically significant.
TABLE 3. INITIAL MEDICAL MANAGEMENT
Secondary hospitals
n
=
43
(%)
TBH
n
=
33
(%)
p
-value
Aspirin
35 (81)
31 (94)
0.9558
150 mg
30 (70)
28 (85)
0.1253
300 mg
5 (12)
3 (9)
0.7209
β
-blocker
15 (35)
22 (67)
0.0055*
Nitrates
25 (60)
17 (56)
0.6559
sub-lingual
16 (40)
9 (30)
0.4046
intravenous
9 (21)
8 (24)
0.7313
Heparin
LMWH
37 (86)
32 (97)
0.0829
UFH
0 (0)
0
(0)
Morphine
7 (16)
4 (12)
0.6071
Dobutamine
6 (14)
1 (3)
0.0829
LMWH: low-molecular weight heparin, UFH: unfractionated heparin.
*
p
-values calculated comparing TBH and secondary hospital groups,
p
<
0.05
was statistically significant.
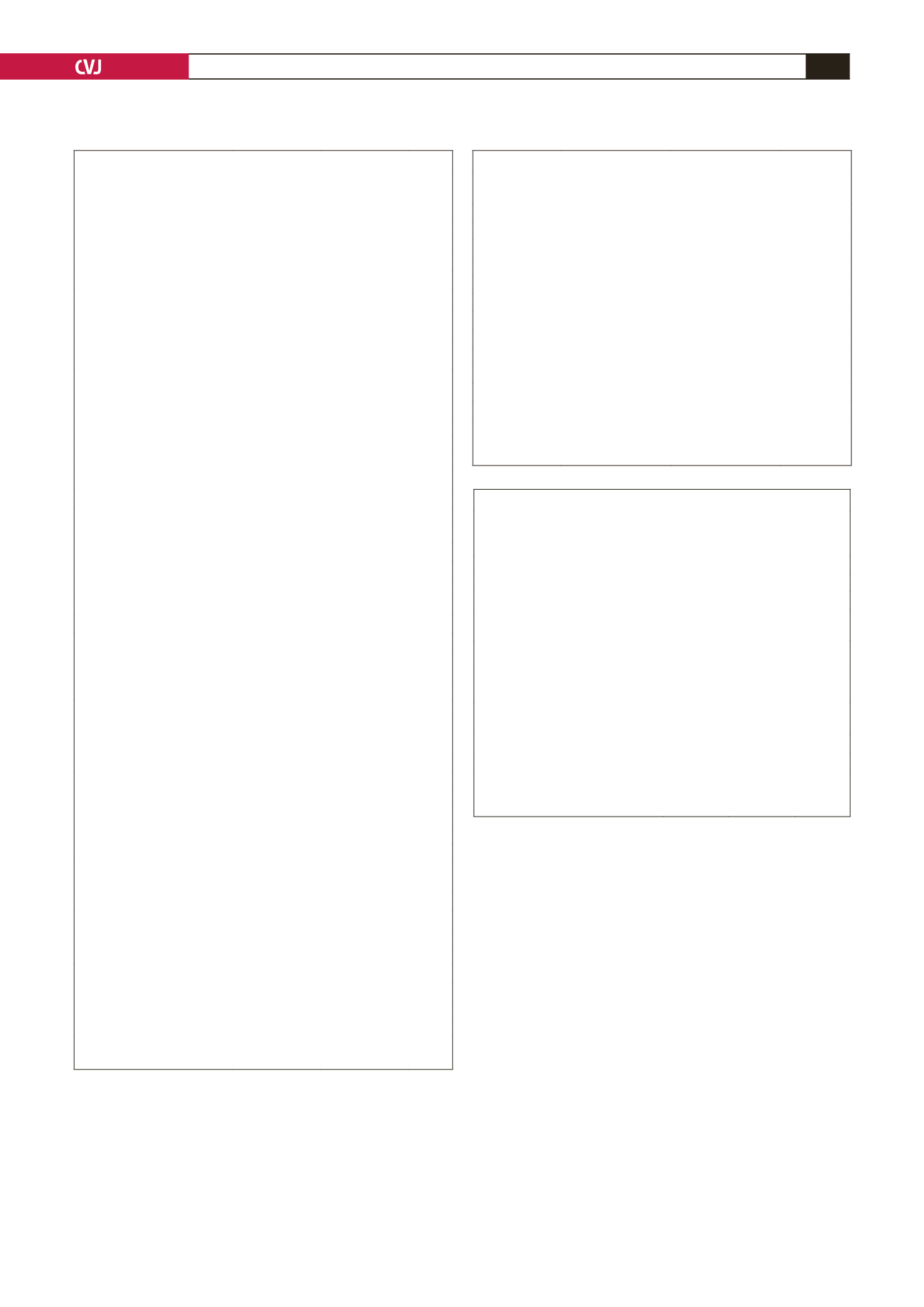
TABLE 2. CLINICAL PRESENTATION
Secondary
hospitals
n
=
43
(%)
TBH
n
=
33
(%)
p
-value
Chest pain
First episode
25 (58)
19 (58)
0.9606
Time to present (hours) (
±
SD) 19.65 (
±
29.54) 30.15 (
±
38.21) 0.1963
Duration of pain (mins) (
±
SD) 30.15 (
±
38.21) 47.58 (
±
35.51) 0.1488
Recurrence
23 (55)
14 (42)
0.2880
Pulse rate (beats per minute)
(
±
SD)
84.16 (
±
28.20) 87.84 (
±
19.89) 0.4072
Systolic blood pressure (mmHg)
(
±
SD)
130.67 (
±
35.84) 144.84 (
±
33.30) 0.0822
Diastolic blood pressure
(mmHg) (
±
SD)
75.90 (
±
19.81) 80.21 (
±
17.91) 0.9568
ECG findings
Normal
2 (5)
2 (6)
0.7859
Previous MI
9 (21)
9 (27)
0.5203
ST depression
19 (44)
16 (48)
0.7094
T-wave changes
Flattening
6 (14%
1 (3)
0.0829
Inversion
10 (23)
11 (33)
0.3315
Dynamic changes
10 (23)
12 (36)
0.2129
Wellens’ syndrome
2 (5)
4 (12)
0.2322
Left ventricular hypertrophy
5 (12)
5 (15)
0.6536
Left bundle branch block (old)
4 (9)
4 (12)
0.6925
Right bundle branch block
6 (14)
4 (12)
0.8142
Atrial fibrillation
3 (7)
2 (6)
0.8727
Atrial flutter
0 (0)
1 (3)
0.2505
Finger-prick blood glucose
(mmol/l)
<
4 .0
1 (2)
0 (0)
0.3779
4.1–6.9
27 (63)
15 (45)
0.1319
7.0–10.0
8 (19)
6 (18)
0.9624
10.1–19.9
7 (16)
10 (30)
0.1459
≥
20.0
0 (0)
2 (6)
0.1018
Temperature (°C)
35.85 (
±
0.61)
36.10 (
±
0.59) 0.0768
Cardiac failure
18 (42)
12 (36)
0.4740
Killip II
8 (19)
5 (15)
0.6919
Killip III
3 (7)
5 (15)
0.2497
Killip IV
7 (16)
2 (6)
0.1718
Serum creatinine (
μ
mol/l)
(
±
SD)
100.09 (
±
35.46) 101.21 (
±
33.75) 0.1938
TIMI score (
±
SD)
3.46 (
±
1.42)
4.33 (
±
1.08) 0.0046*
GRACE score (
±
SD)
Probability of death
in hospital
8.79 (
±
14.60)% 5.49 (
±
0.09)% 0.2321
at 6 months
15.57 (
±
22.49)% 11.03 (
±
12.68)% 0.2695
Probability of death or MI
in hospital
18.81 (
±
12.82)% 16.72 (
±
8.94)% 0.4279
at 6 months
31.67 (
±
19.59)% 28.39 (
±
13.36)% 0.4119
*
p
-values calculated comparing TBH and secondary hospital groups,
p
<
0.05
was statistically significant.