CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 4, May 2013
138
AFRICA
Results
Video-assisted thoracoscopic sympathectomies (670) were
performed in 335 patients with severe primary hyperhydrosis
(Table 1). Of the 113 patients, 57.31% (
n
=
192) were female,
42.69% (
n
=
143) were male, and the mean age was 28.32 (range
18–54) years. Palmar and axillary hyperhydrosis were the most
common symptoms. Hyperhydrosis was observed in the palmar
and axillary region in 175 (52. 23%) patients, only in the palmar
region in 52 (15.52%), in the craniofacial region in 44 (13.13%),
only in the axillary region in 42 (12.53%), and in the palmar and
pedal regions in 22 (6.56%) patients.
Bilateral video-assisted thoracoscopic sympathectomy was
performed in all patients. T2 resection was performed in 44
patients with craniofacial hyperhydrosis. T3 resection was
performed in 94 patients with only palmar and only axillary
hyperhydrosis. T3–T4 resection was performed in 175 patients
with palmar and axillary hyperhydrosis. T3–T5 resection was
performed in 22 patients with palmar and pedal hyperhydrosis.
The mean operating time was 51 (range 37–78) minutes.
Re-operation required for 3 (0.89%) patients due to bleeding.
Usually, patients were discharged within 24–48 hours after
operation. The mean follow-up period was 24 (range 6–48)
months. Most of the patients presented with an improvement in
primary hyperhydrosis. The initial cure rate was 95% and the
initial satisfaction rate was 93%. There was no mortality in this
study. No recurrence was reported at the follow-up period. The
complication rate was 15.82% in 53 patients. Compensatory
sweating was the most frequent complication in 34 (10.14%)
patients.
Discussion
Primary hyperhydrosis is a disorder characterised by excessive
sweating. Somewhat more frequent in women, there is an
obvious family predisposition and its incidence is higher in
certain populations (Asians and Sephardic Jews), representing
1% of the population.
3
The condition is bilateral, symmetrical
and is sometimes related to or exacerbated by emotional or
seasonal situations. Although there are generalised forms, focal
hyperhydrosis is the most frequent presentation. Palmar and
axillary hyperhydrosis are the most common, followed by plantar
hyperhydrosis.
Although its pathophysiology is unclear, it is believed to be
caused by hyper-stimulation or over-activity of the sympathetic
nervous system that passes through the upper thoracic ganglia.
1
The diagnosis of primary focal hyperhydrosis is based on
symptoms, and supported by a specific clinical history. Help is
needed to distinguish focal from generalised hyperhydrosis. The
Multi-Specialty Working Group on Hyperhydrosis in the United
States has proposed some criteria for the diagnosis of focal
hyperhydrosis (Table 2).
4
Although not life-threatening, hyperhydrosis causes
educational and occupational difficulties, as well as psychological
and social problems. Medical treatment is often unsuccessful and
the response is usually transient. Therapeutic options for its
management include topical anti-perspirants, anti-cholinergic
drugs, iontophoresis and recently, botulinum toxin injections.
5,6
Interruption of the sympathetic innervation of the ecrine
sweat glands via the upper thoracic ganglia during surgery is
the best procedure for hyperhydrosis. Surgery of the thoracic
sympathetic nervous system has been performed since the
beginning of the 20th century.
7
Thoracoscopic sympathectomy
was first described in 1942 by Hughes, and remained rare until
the introduction of video-endoscopic techniques in the 1980s.
8
Since then it has become the preferred method of treatment of
primary hyperhydrosis of the palms, axillae, and more recently
for facial blushing. Its popularity has grown so much that the
technique is now used around the world.
Bilateral endoscopic sympathectomy can be performed by
different surgical and anaesthesiological techniques. Giving
the patient the chance to achieve both functional and aesthetic
results with minimal risk and discomfort, together with an
excellent postoperative quality of life is the gold standard.
9
Different techniques are used for intra-operative ventilation
of these patients. Orotracheal intubation with a double-lumen
endotracheal tube is most commonly used but there are reports
of the use of ventilation with a laryngeal mask, as well as surgery
under sedation with spontaneous ventilation, with satisfactory
results.
10
In recent years, numerous articles advocating diverse surgical
techniques (ablation, resection, interruption by clips, etc) for
accessing the thoracic sympathetic chain have been published.
Hashmonai
et al
. compared surgical techniques for the treatment
of hyperhydrosis (resection or electrocoagulation) based on
a review of the studies published between 1974 and 1999.
11
Although resection seems to provide better results, the authors
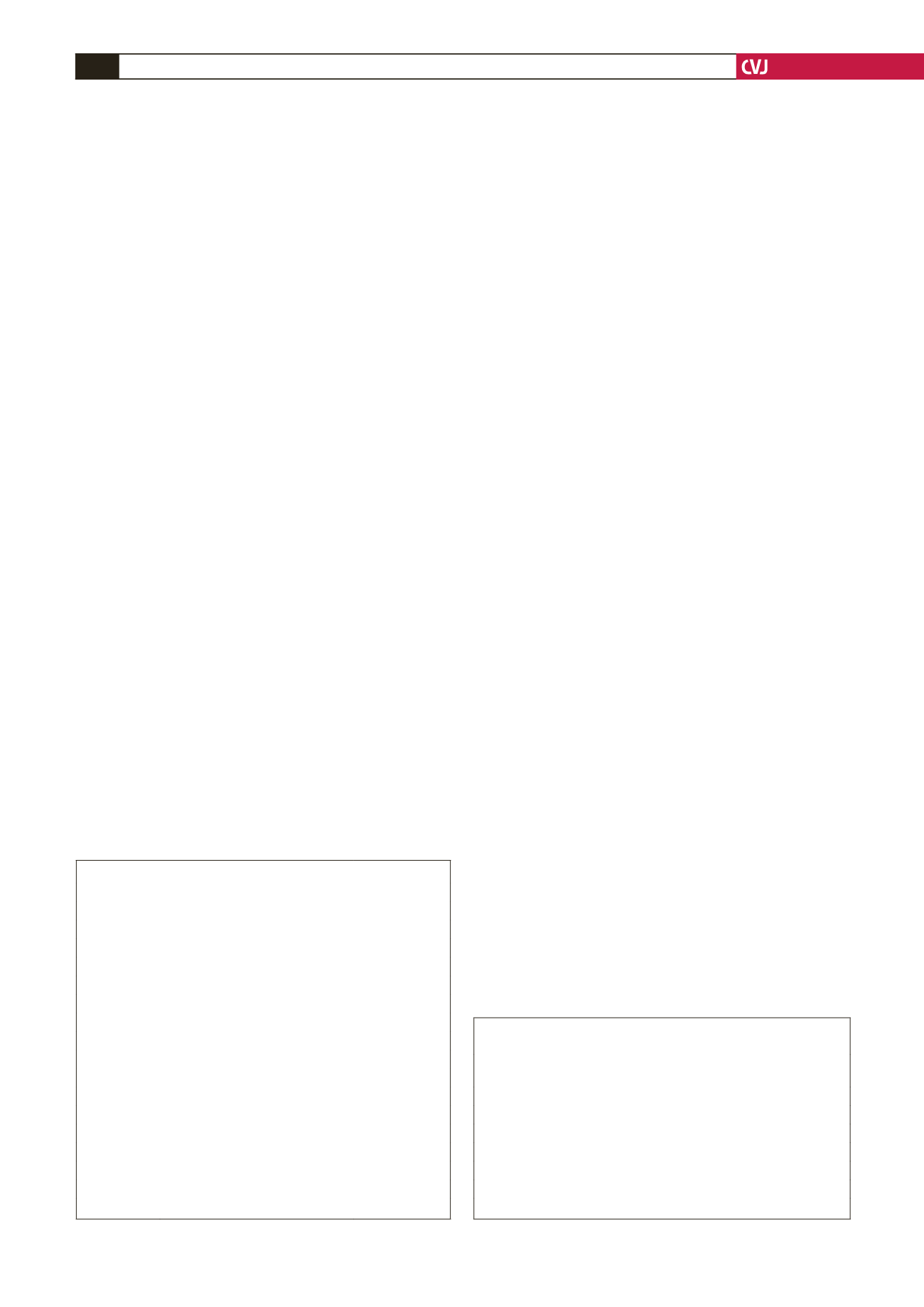
TABLE 2. CRITERIA FOR PRIMARY FOCAL
HYPERHYDROSIS DIAGNOSIS
A Focal, visible, excessive sweating for a period of at least six months
with no known secondary cause
B At least one of the following characteristics:
• bilateral and symmetrical
• frequency of at least one episode per week
• interferes with daily activities
• presentation before the age of 25
• family history
• cessation of excessive sweating during sleep.
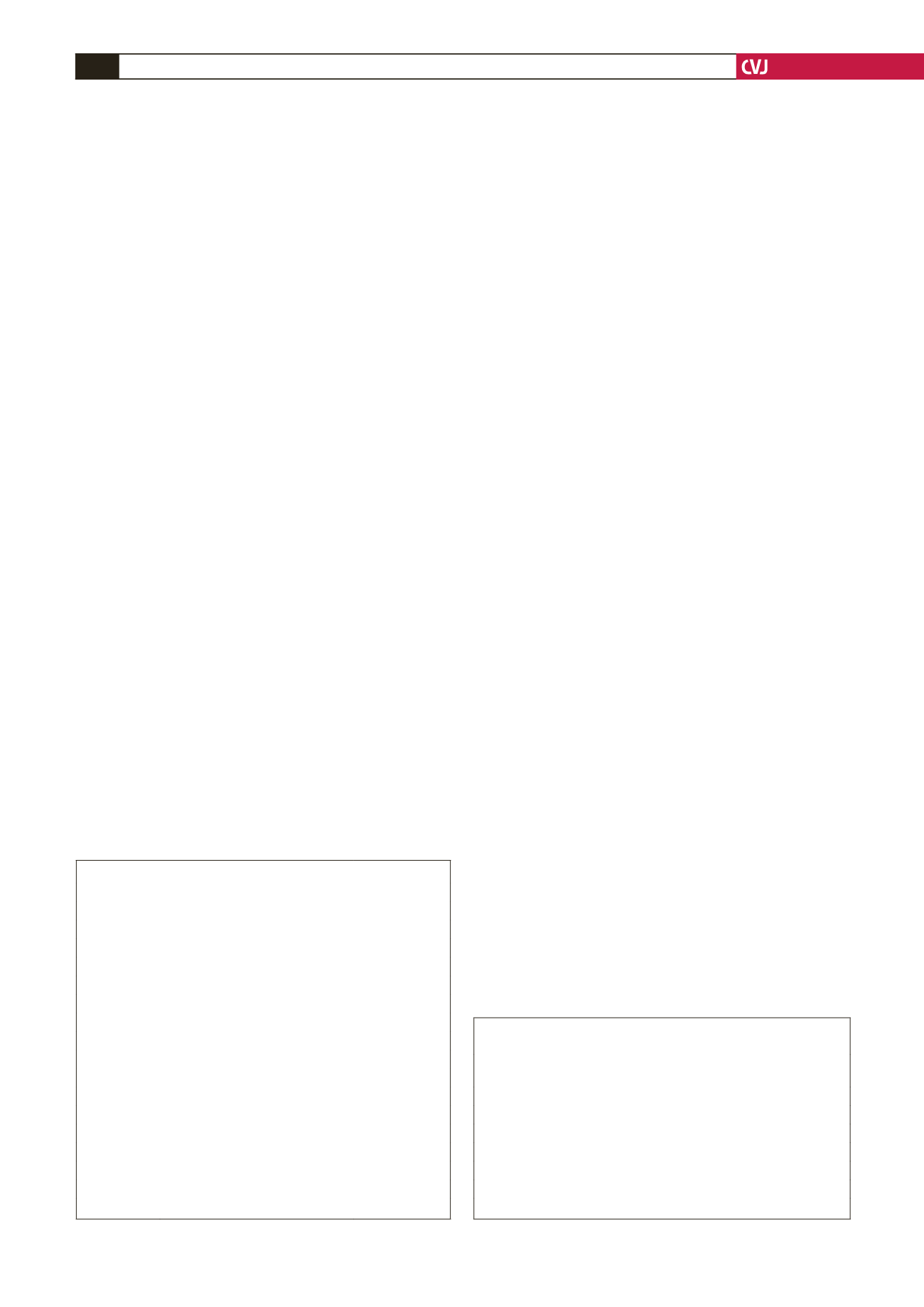
TABLE 1. PATIENTS CHARACTERISTICS
Mean age
28.32 (range 18–54) years
Gender
Male
42.69% (
n
=
143)
Female
57.31% (
n
=
192)
Localisation of
hyperhydrosis
Palmar and axillary (T3–T4 resected) 52.23% (
n
=
175)
Isolated palmar (T3 resected)
15.52% (
n
=
52)
Craniofacial (T2 resected)
13.13% (
n
=
44)
Isolated axillary (T3 resected)
12.53% (
n
=
42)
Palmar and pedal (T3–T5 resected)
6.56% (
n
=
22)
Complications Compensatory sweating
10.14% (
n
=
34)
Hyperesthesia at the incision area
2.08% (
n
=
7)
Pneumothorax
1.49% (
n
=
5)
Bleeding
0.89% (
n
=
3)
Horner’s syndrome
0.59% (
n
=
2)
Emphysema
0.29% (
n
=
1)
Chylothorax
0.29% (
n
=
1)
Re-operation 0.89% (
n
=
3)
Recurrence
0
Mortality
0