CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 4, May 2013
e8
AFRICA
Oral food intake was ceased and total parenteral nutrition
(TPN) was initiated for two weeks. After the second week, TPN
was stopped and his diet was changed to a high-protein one
containing medium-chain triglycerides for 10 days. However on
the second day, the drainage tailed dramatically to 50 ml/day.
The drainage fluid was completely chylous and the patient
had a milky chylous drainage for 24 days, producing 50 ml
of drainage daily. The chylous leak continued to diminish in
volume, with no drainage by the last five days. The patient
was subsequently put on a normal diet. The drain output was
observed closely for five days after re-institution of the normal
diet. There was no further chylous leak.
An echocardiogram confirmed no re-accumulation in the
pericardial space and the drain was therefore removed and the
patient discharged uneventfully. Clinical and echocardiographic
follow up at four weeks showed no recurrence of pericardial
fluid.
Discussion
Chylopericardium after intra-thoracic surgery is rare. Thomas and
McGoon reported the first case of a chylous pericardial effusion
following cardiac surgery.
1
The most common causes are trauma
(blunt or penetrating), thoracic or cardiac surgery (especially for
congenital heart disease) and congenital lymphangiomatosis.
Thymus gland injury is reported mainly in the paediatric
literature as a cause of chylous pericardial effusion, because
the thymus gland involutes after adolescence. This particular
complication becomes rare in the adult population, with most
of the literature consisting of single case reports. These include
chylopericardium after aortic valvotomy, repair of tetralogy of
Fallot and coronary artery bypass graft surgery.
2,3
Chylopericardium may also be the result of explorative
procedures during the preparation of patients for surgery. Over-
retraction of the chest wall may harm the lymphatic channels
where the ductus thoracicus drains. Encircling of the inferior
vena cava during the cannulation procedure may cause lymphatic
leakage due to damage of the lymph channels. Lymphatic
channels around the thymus may be damaged during surgical
exploration. Cauterised perithymic and intrathymic lymphatics
may cause postoperative chylous leakage if the thymus lobes
were not blunt dissected and ligated.
4
Chylous drainage may occur in the early and late period
following cardiac surgery. Early chylopericardiumis characterised
by a progression in serious drainage and the colour changes to
white-yellow after the start of fatty oral intake. Late-onset
chylopericardium comes with signs of cardiac tamponade that
causes increased cardiac silhouette, prominent neck veins and
palpable liver. This may change from the first postoperative day
to the post-discharge period.
Diagnosis and treatment of patients who develop a
chylopericardium vary. The chylous pericardial fluid is a sterile,
milky, odourless fluid containing microscopic fat droplets and
is alkaline with a density of 1 010–1 020 mg/dl.
5
The presence
of fat globules in a Sudan III stain of the drainage fluid helps to
diagnose the cyhlous nature. In late-onset symptomatic cases, the
condition may be diagnosed with the help of telecardiography
and echocardiography.
In our case, the symptoms began 10 days after discharge,
with normal oral nutrition. The patient was diagnosed with
echocardiography as cardiac tamponade. Chylopericardium
was diagnosed macroscopically after pericardiosynthesis and
confirmed with biochemical analysis of the fluid.
Treatment may be conservative or surgical in patients with
chylous drainage. In early cases, follow up of the mediastinal
drainage and changing the patient’s diet to TPN that is rich in
medium-chain fatty acids is generally accepted.
6
In late-onset
cases with signs of pericardial tamponade, pericardiosynthesis,
re-insertion of a mediastinal drain or surgical ligation of
the ductus thoracicus may be the treatment options.
5
Also,
somatostatin infusion has been shown to decrease the drainage.
7
Surgical ligation is advised in cases with daily drainage amounts
of more than 1 500 ml, unchanged amounts of drainage for more
than 14 days or in patients with nutritional complications.
8
The management strategy for non-responding patients is a
dietary modification, and later a TPN regimen within the first
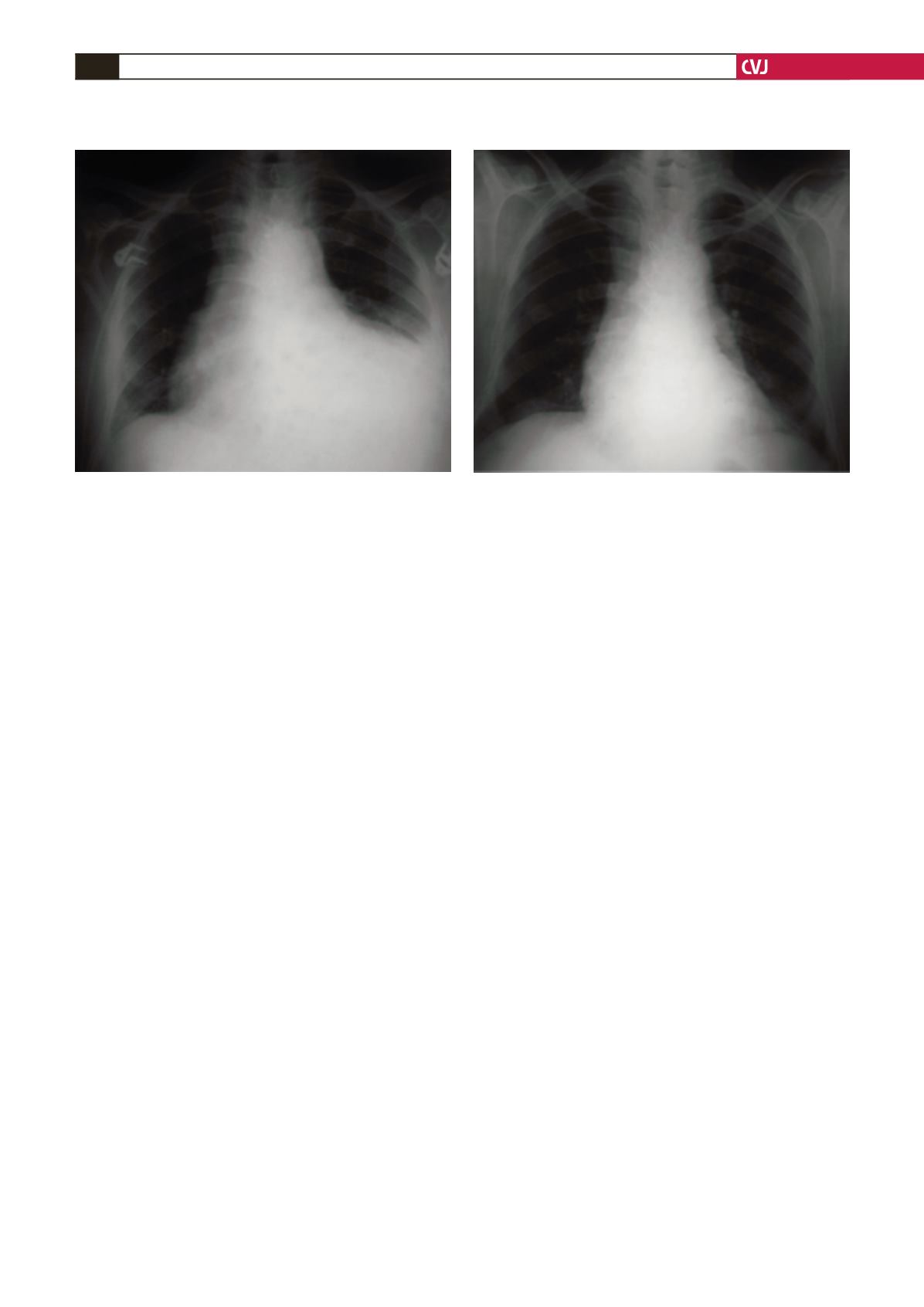
Fig. 1. Chylopericaridum after mitral valve and coronary
artery bypass surgery. PA chest radiograph showing peri-
cardial effusion and cardiomegaly.
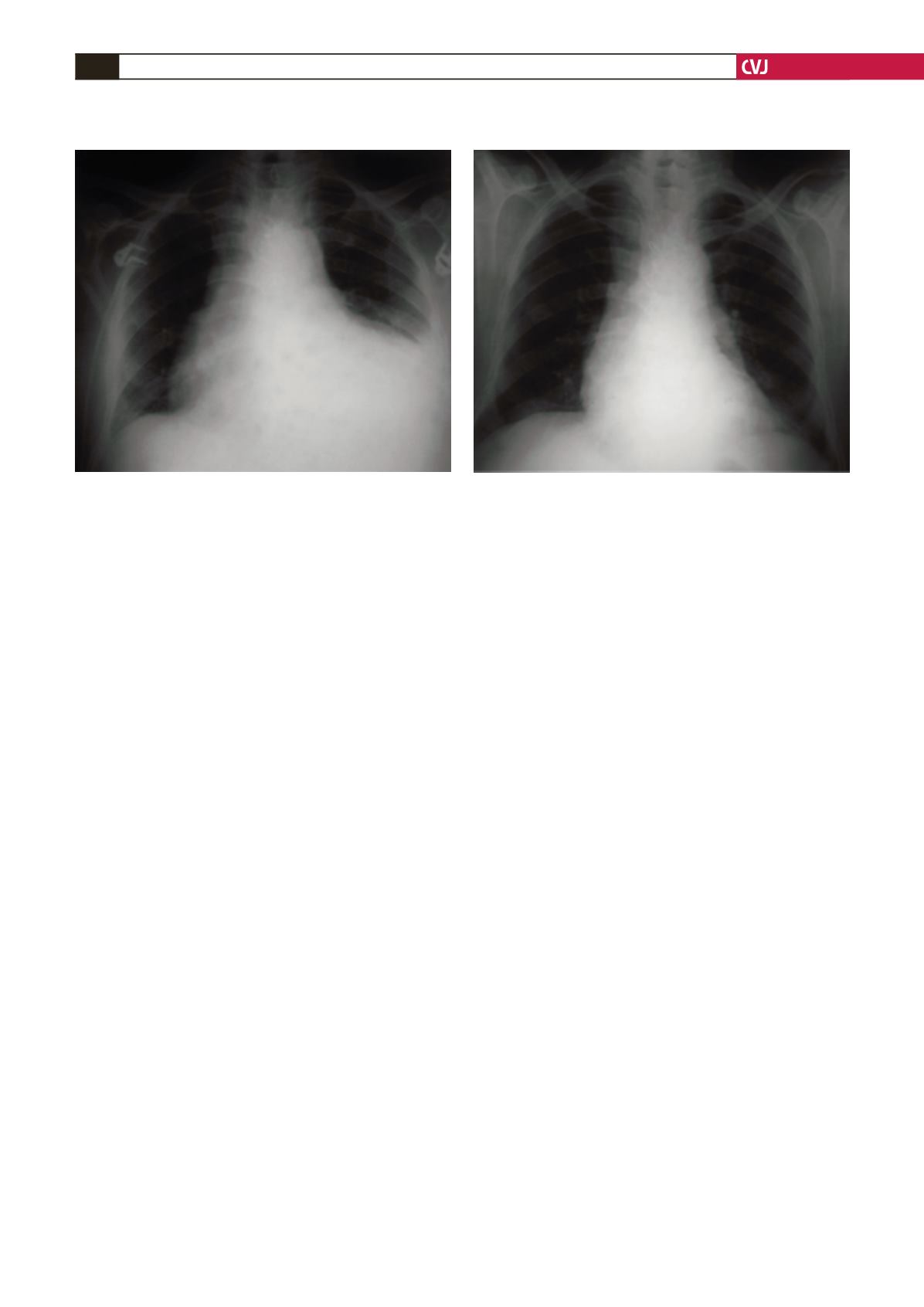
Fig. 2. PA chest radiograph of patient after treatment.