CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 4, May 2013
AFRICA
e5
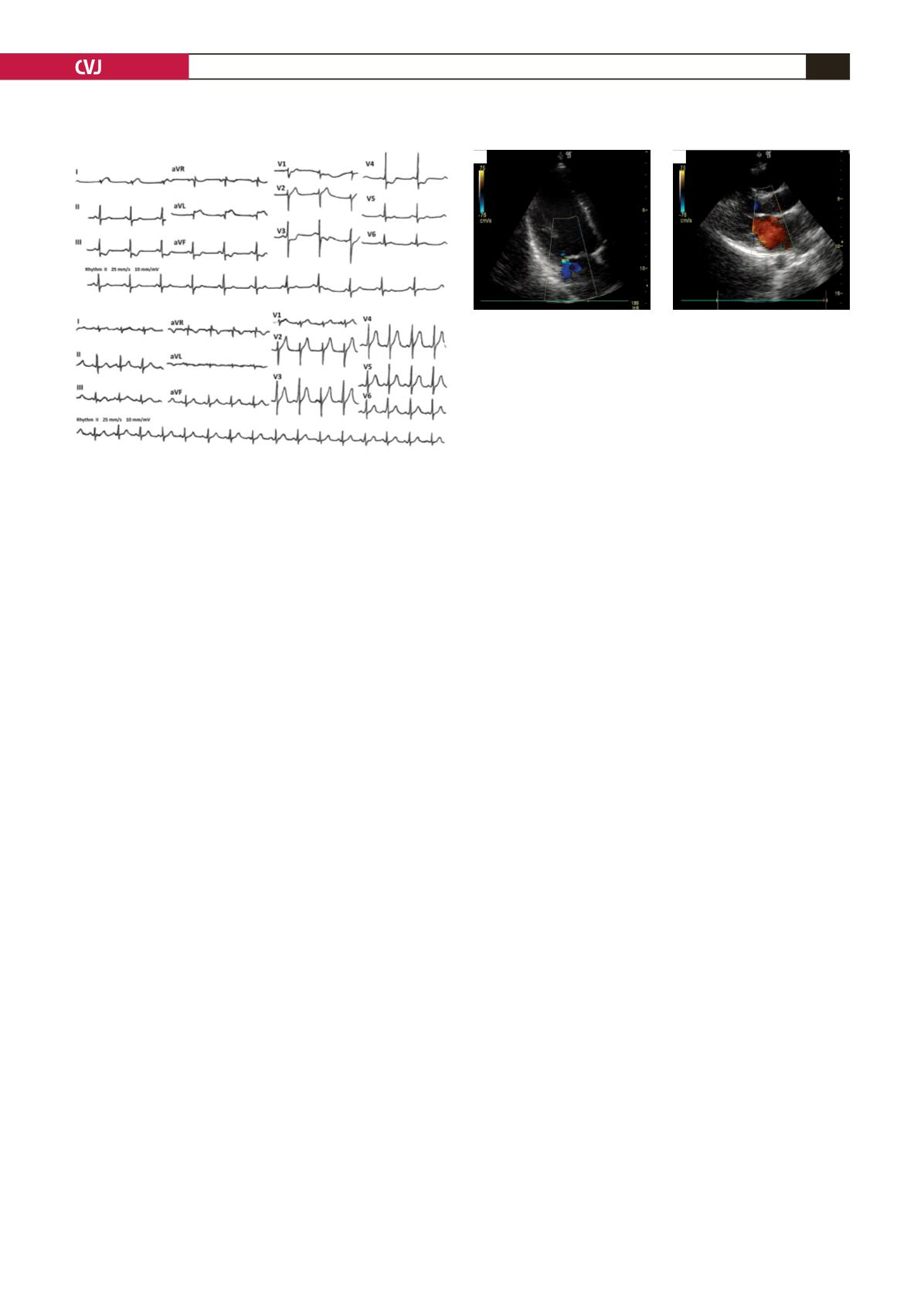
1b). The wall movement abnormalities were limited to the
posterior wall only and mitral regurgitation disappeared in two
hours, as seen on the control echo (Fig. 2b). The cardiac enzyme
levels had increased about two-fold in the sixth hour from that of
baseline [creatinine kinase (CK-MB): 42 U/l (22 U/l at baseline;
n
<
25 U/l), troponin I: 3.12 ng/ml (0.01 ng/ml at baseline;
n
=
0–2.00 ng/ml)].
Because no coronary intervention facility existed closer than
three hours away and the patient had stabilised in a short time,
transferral of himwas delayed for 10 days, for recovery. Coronary
angiography showed no evidence of obstructive coronary artery
disease. Intravascular ultrasound imaging (IVUS) (Atlantis 40
mHz, Boston Scientific Co, USA) also clearly demonstrated no
evidence of coronary artery disease. An allergic stimulation test
was not performed because the patient refused approval.
Discussion
An allergic reaction following a wasp sting has a wide spectrum
varying from local reactions to anaphylaxis. Severe anaphylaxis
may induce bronchospasm, profound vasodilation and angio-
oedema. Underlying subclinical coronary atherosclerosis may
also become clinically evident.
Cardiac involvement is an uncommon but important clinical
finding with these conditions. There have been some such
cases in subjects with normal coronary arteries,
1-6
and in
subjects with coronary artery disease.
7-9
Some originated from
the anaphylaxis itself,
4,8,9
or from drugs used for its treatment,
including epinephrine
1-3,5-7
The use of epinephrine to counteract possible systemic
reaction in anaphylaxis has been revealed to cause MI.
1,3
Although chlorpheniramine maleate rarely causes mild
ventricular depression and transient bradytachycardia (if the
administration is too fast), there is no known incidence of MI due
to prednisolone or chlorepheniramine maleate administration in
the literature.
The main mechanism proposed is vasospasm of the coronary
arteries. Other mechanisms, such as plaque activation and
systemic hypotension, may play a role in its pathogenesis.
Hypotension may lead to global ischaemia in the heart rather
than local myocardial infarction, therefore diffuse ST depressions
with ST elevation in the aVR would have been evident.
An hypothesis of the central role of mast cells, inflammatory
cell activation and release of potent vasoactive mediators, called
cardiac anaphylaxis, is also suggested.
8
Kounis syndrome or
allergic MI is defined as resulting in coronary vasospasm, which
is mediated by vasoactive amines released by mast cells, and
patients may also have eosinophilia.
12
The chemical composition
of wasp venom basically consists of vasoactive amines and
thrombogenic substances that are able to create vasospasm, and
coronary thrombosis may play a role in the pathophysiological
determination.
Clinically, anaphylaxis may induce an acute ischaemic burden
due to a combination of reduced coronary perfusion pressure,
tachycardia, and sometimes severe hypoxia. This combination
of events may hamper adequate cardiac response to the extreme
vasodilation, and even lead to reduced cardiac output and further
deterioration. MI during the course of the allergic reaction in
the absence of systemic hypotension has rarely been reported.
13
However, our patient’s blood pressure was not low, so it was
not hypotension-induced myocardial infarction in our case. In a
similar case, the possibility of severe coronary spasm associated
with anaphylactic reaction was considered, even though other
symptoms were mild or absent.
7
Local histamine release seems to induce spasm of the
coronary vasculature, thus leading to myocardial ischaemia and
infarction. Eosinophilic basic proteins or vasoactive cytokines
may directly stimulate constriction of nearby smooth muscle.
Eosinophilic infiltration has been shown around the vasa
vasorum and nerve fibres.
14
Stimulation of these nerve fibres in
the adventitia is another possible explanation for the vasospasm.
ST elevation was seen in the majority of cases of vasospasm
associated with eosinophilia, similar to prinzmental angina.
15
Vasospasm-related symptoms may continue despite high-dose
vasodilators but respond well to prednisone.
Corticosteroids may be speculated to have some role on the
cardiovascular response. Owecki
et
al.
11
presented a case of a
woman who received high doses of methylprednisolone (1 g iv
daily) for active Graves’ ophthalmopathy. Severe hypertension
developed, followed by myocardial infarction on the fifth day
of treatment, but in this case, the drug dose was high and
hypertension played the major role in developing the MI.
On the other hand, a Löffler’s endocarditis associated with
unusual ECG change mimicking posterior myocardial infarction
was succesfully treated with prednisolone.
16
Azar
et
al.
reported
a 48-hour course of anti-inflammatory therapy with methyl
prednisolone did not change the short-term outcome of patients
A
B
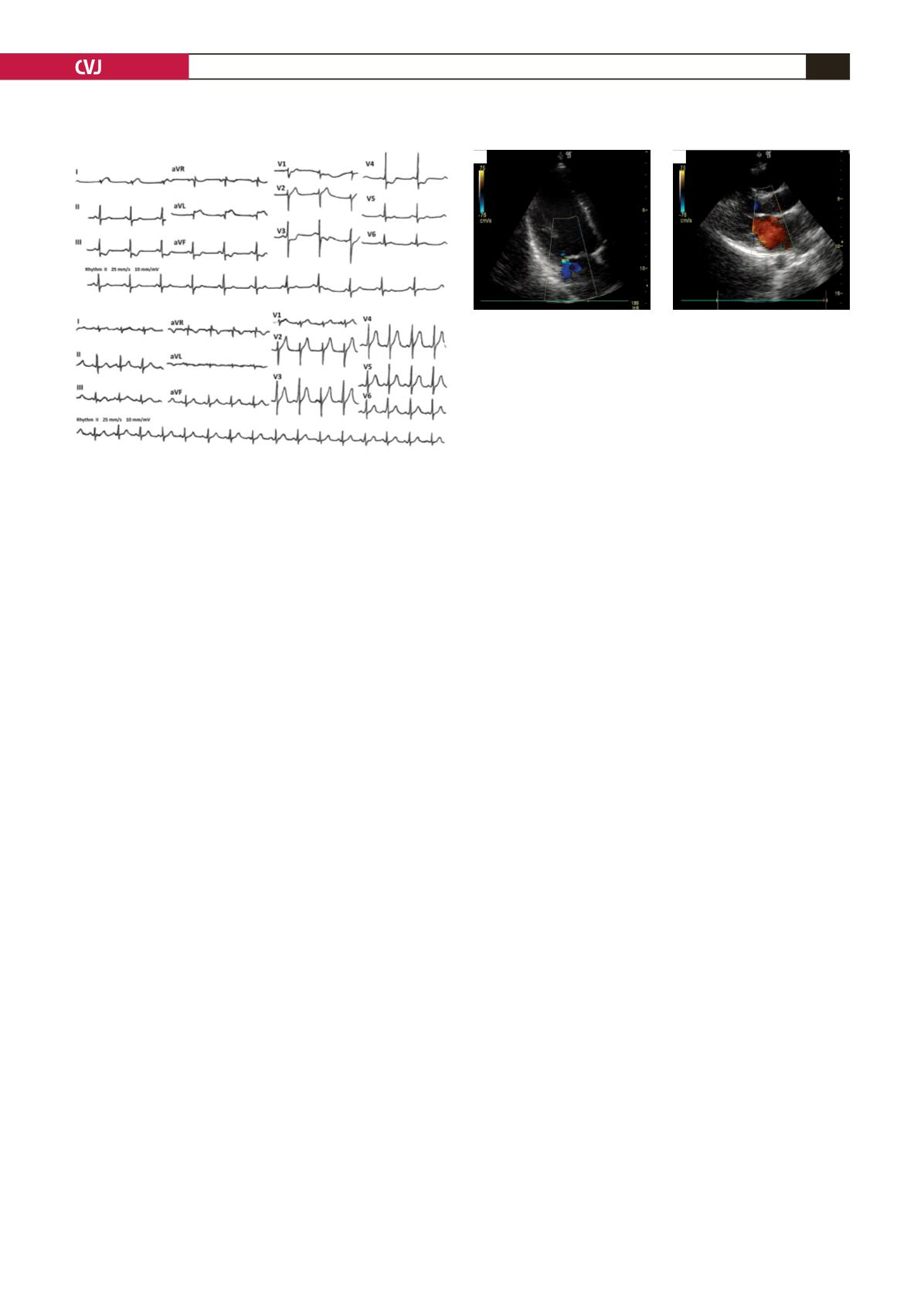
Fig. 1. A. ECG shows ST elevation with a reciprocal
depression. B. After 25 min the ST deviations resolved.
A
B
Fig. 2. A. Echocardiography shows left ventricular poste-
rior, lateral and apical wall movement abnormalities and
mild mitral regurgitation. B. Control echo after 2h shows
posterior wall movement abnormalities only.