CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 5, June 2013
158
AFRICA
error.
19,20
Therefore, new methodologies that can evaluate LA
function by analysis of LA myocardial deformation may be of
potential clinical interest.
Two strain imaging methods are based on different principles
and can potentially give different results. Tissue Doppler imaging
(TDI)-derived strain is limited to the measurement of movement
parallel to the ultrasound beam. Non-Doppler 2D strain imaging
derived from speckle tracking is a newer echocardiographic
technique for obtaining SR measurements. The advantage of this
method is that it tracks in two dimensions, along the direction
of the wall, not along the ultrasound beam, and thus is angle
independent, which is a great advantage of non-Doppler 2D
strain imaging in comparison to TDI-derived strain data.
2
Previous studies show that 2D STE with its latest applications
such as strain rate imaging may represent promising techniques
to better evaluate LA function.
21
With the use of strain rate
imaging, Inaba
et al.
found that SRs corresponded to reservoir
function and SRe corresponded to conduit function, while SRa
corresponded to booster pump function.
22
In patients with AMI, left ventricular stroke volume is
relatively maintained despite the impairment of left ventricular
function caused by myocardial ischaemia and necrosis. With
increased stiffness or reduced compliance of the LV, LA pressure
rises to maintain adequate LV filling, and the increased atrial
wall tension leads to chamber dilatation and stretch of the atrial
myocardium.
23
Therefore, the left atrium works harder and
transports more blood to the left ventricle during left ventricular
diastole. This function of the left atrium can be attributed to the
Frank-Starling mechanism. LA pump function augmentation is
therefore due to the increased left atrial volume before active
atrial emptying, but not to the increased contractility of the left
atrium.
24
In our study protocol, patients with NSTEMI showed
increased LA volumes (LAV
max
, LAV
min
and LA
p
). Moreover,
indices of LA reservoir function (LA total EF) and LA conduit
function (LAPEF) were significantly impaired and compared
with healthy controls, but LA booster function (LAAEF) seemed
to be unchanged in both normal subjects and patients (Table 2).
In accordance with the conventional echocardiographic
parameters mentioned above, we found LA reservoir function
assessed by SR imaging (LA-GLSRs) and LA conduit function
assessed by SR imaging (LA-GLSRe) were significantly reduced
in patients with NSTEMI (Table 4), but LA booster function
assessed by SR imaging (LA-GLSRa) showed no significant
difference. This may be explained by when the LA is well
stretched longitudinally, and consequently a high LA positive
peak is present, the LV then relaxes rapidly, generating a high E
wave, as blood rushes into the LV, generating a high passive LA
emptying fraction. Therefore, LA-GLSRs and/or LA-GLSRe
have significant correlations with LV diastolic function, which
are impaired in patients with NSTEMI.
In our study protocol, a good correlation was found between
LA global strain rate and LA functional parameters (Table 5).
The present study extends previous results and describes changes
in LA function after AMI, combining LA volumes, LA emptying
fraction, and LA strain in patients with NSTEMI. The results
show that speckle tracking-derived strain rate is a promising
technique to assess LA function as well as LA volumes and LA
emptying fraction.
Global strain is a relatively new parameter for assessment of
LV function
25
and tends to predict the infarct mass better than
established indices of global function such as LVEF and WMSI.
LVEF can be regarded as the sum of all LV systolic deformation.
InWakami
et al
.’s study, peak LA strain rate during LV systole,
which corresponds to our measured LA-GLSRs, correlated
inversely with LV end-diastolic pressure and LV end-systolic
volume and positively with LVEF.
26
In a recent study by Vartdal
et al
., global strain measured by TDI immediately after PCI was
found to be superior to LVEF for predicting final infarct mass
in patients with acute MI.
27
Comparing with tagged magnetic
resonance imaging (the current ‘gold standard’ for deformation
analysis), STE measurements correlated well with data obtained
by magnetic resonance imaging, both in normal myocardial
segments and infarcted areas (
r
=
0.87,
p
<
0.001).
28
The findings of our present study are in accordance with
previous studies. There was significant correlation between LVEF
and global LA-GLSRs (
r
=
–0.334,
p
<
0.05) or LA-GLSRe (
r
=
–0.477,
p
<
0.001). In particular, LA-GLSRe was strongly
correlated with LV-GLSRe (
r
=
–0.644,
p
=
0.001), while
LA-GLSRs and LA-GLSRa were not significantly correlated
with LV strain rate parameters (LV-GLSRs and LV-GLSRa).
These findings support the idea that LA-GLSRe can serve as an
important new marker of LA and LV function in the acute MI.
Therefore, speckle tracking echocardiography was found to
be a feasible and reproducible method to assess LA longitudinal
strain in healthy subjects and patients with NSTEMI. The
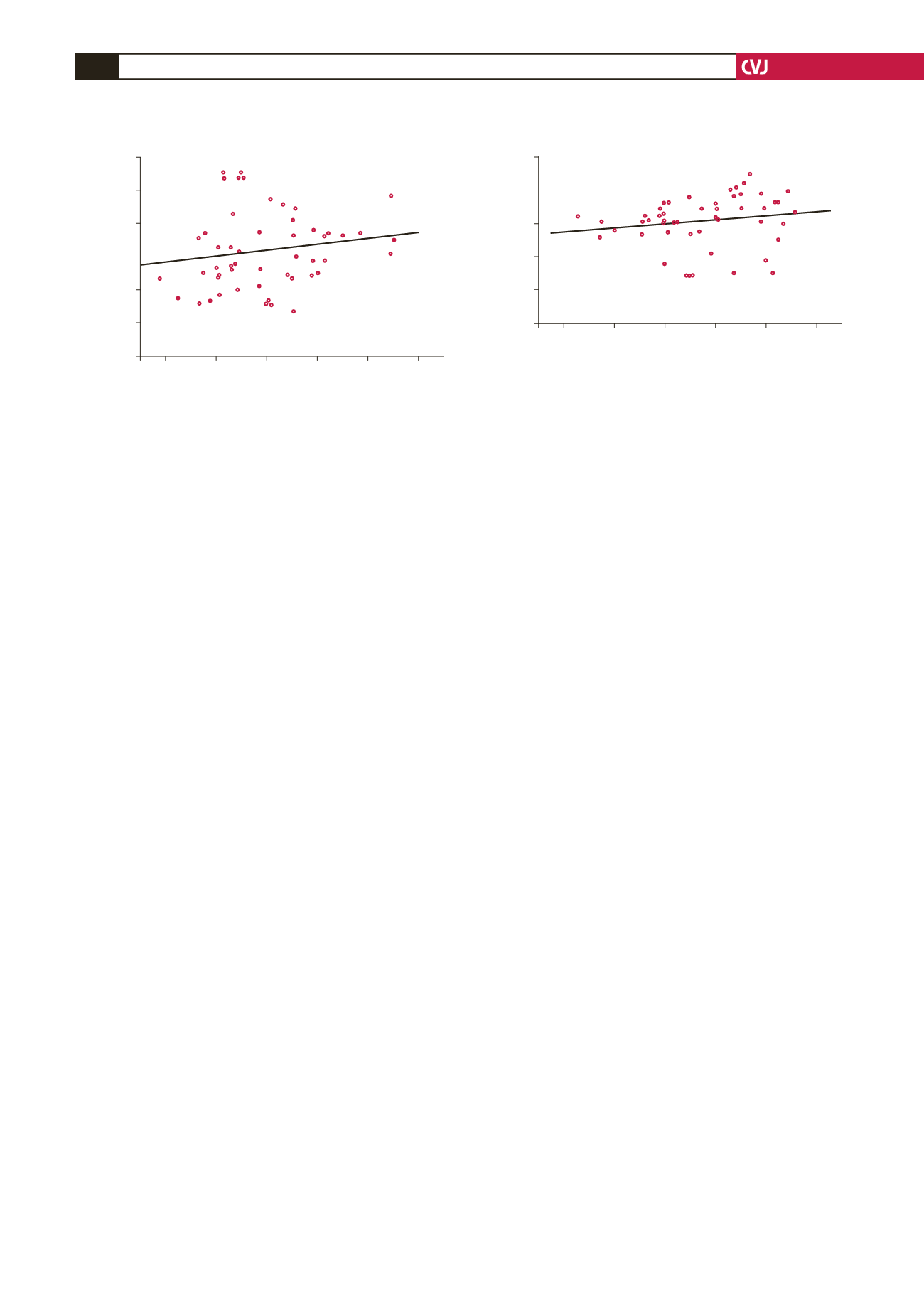
Fig. 7. Correlation between peak early diastolic strain rate
of the left ventricle (LV-GLSRs) and peak early diastolic
strain rate of the left atrium (LA-GLSRs) in patients with
NSTEMI.
3.00
2.50
2.00
1.50
1.00
0.50
–1.20 –1.00 –0.80 –0.60 –0.40 –0.20
LA-GLSRs
LV-GLSRs
r
=
0.234,
p
=
0.098
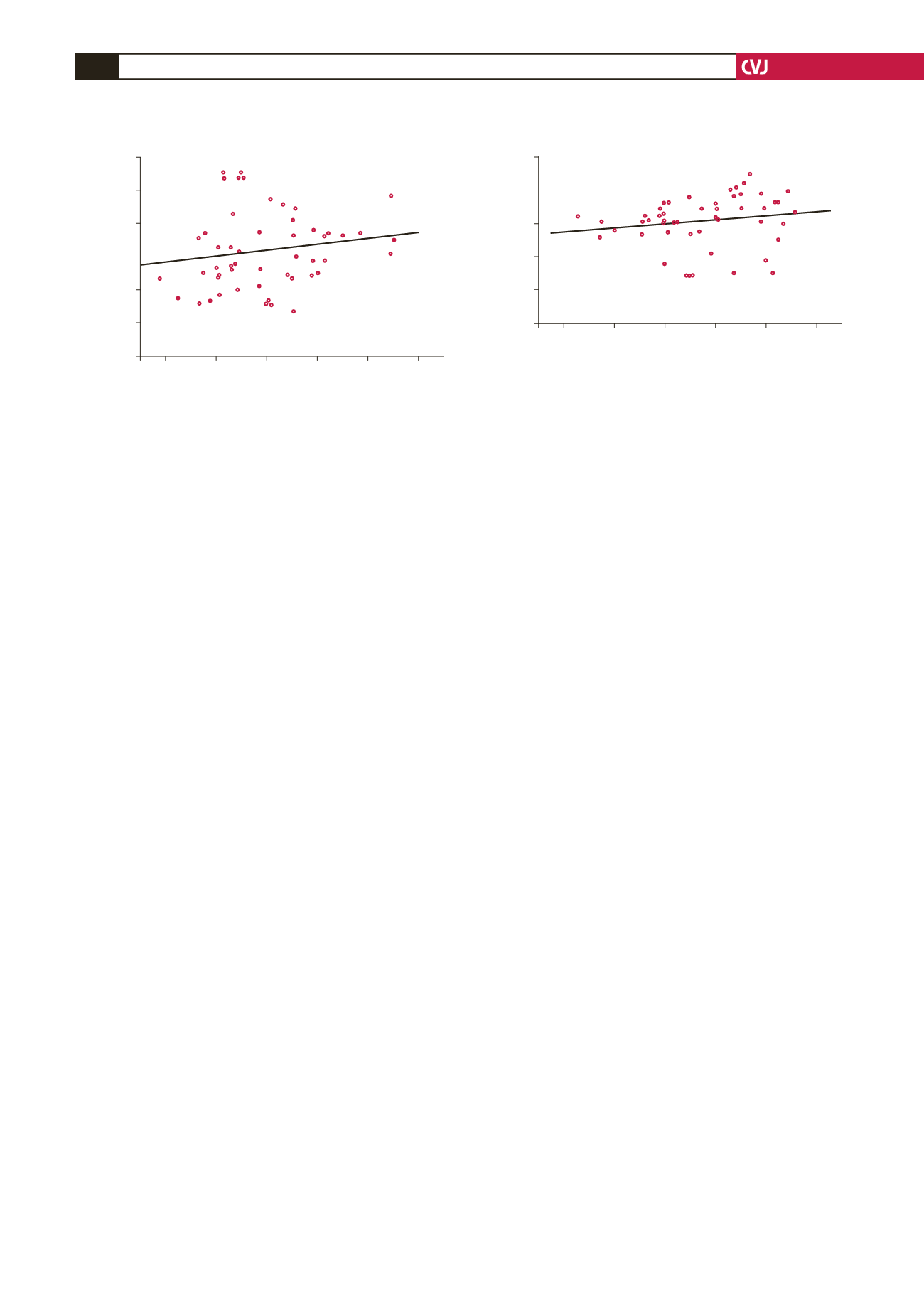
Fig. 8. Correlation between peak early diastolic strain rate
of the left ventricle (LV-GLSRa) and peak early diastolic
strain rate of the left atrium (LA-GLSRa) in patients with
NSTEMI.
0.00
–1.00
–2.00
–3.00
–4.00
0.20
0.40 0.60 0.80 1.00 1.20
LA-GLSRa
LV-GLSRa
r
=
0.266,
p
=
0.059