CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 5, June 2013
AFRICA
167
discharge, all patients received aspirin and clopidogrel, and there
was no statistical difference in percentage use of
β
-blockers,
ACEIs, ARBs, diuretics and statins between the two groups.
The baseline angiographic and procedural characteristics
of the study population are listed in Table 2. With regard to
the extent of coronary artery disease (CAD), the proportion of
multi-vessel disease was similar between the two groups [RG vs
NRG; 41.6% (
n
=
17) vs 42.9% (
n
=
37),
p
=
0.79]. In the RG,
the most frequently involved coronary artery was the left anterior
descending artery [RG vs NRG; 61.9% (
n
=
26) vs 42.7% (
n
=
38),
p
=
0.04].
Almost 90% of patients who underwent primary PCI received
drug-eluting stent (DES) implantation. No difference was
observed in terms of the proportion of DES or bare-metal stent
(BMS) implantation between the two groups. Compared with
a zotarolimus-eluting stent (ZES), we mainly used a sirolimus-
eluting stent (SES) and paclitaxel-eluting stent (PES).
In addition, the final thrombolysis in myocardial infarction
(TIMI) grade 3 flow after primary PCI [RG vs NRG; 85.7%
(
n
=
36) vs 94.4% (
n
=
84),
p
=
0.09] and the number of stents
per patient (RG vs NRG; 1.25
±
0.53 vs 1.27
±
0.36,
p
=
0.33)
showed no significant differences between the two groups. We
seldom used 2b/3a glycoprotein inhibitors during primary PCI
[RG vs NRG; 9.5% (
n
=
4) vs 7.9% (
n
=
7),
p
=
0.78].
Baseline and follow-up haemodynamic parameters as well as
diastolic dysfunction of the study population are listed in Table
3. Mean baseline LVESV and E/E
′
were significantly higher
in the RG than in the NRG. Also, mean baseline LVEF was
significantly reduced in the RG. Follow-up echocardiography
was performed at a mean of 6.5
±
1.1 months after primary PCI.
At the six-month follow up, LVESV and LVEDV in the RG
were increasing compared with baseline values. Mean six-month
follow-up LVEF did not show notable changes compared
with baseline. Although baseline diastolic dysfunction was
not significantly different between the two groups, six-month
follow-up diastolic dysfunction in the NRG showed a notable
improvement. Mean six-month follow-up E/E
′
in the RG was
decreased in both groups, but mean E/E
′
was significantly higher
in the RG (RG vs NRG; 11.2
±
6.2 vs 7.9
±
3.8,
p
<
0.01).
Mean time of plasma BNP measurements in the early phase
was 2.8
±
0.5 days, in the late phase 3.7
±
0.6 weeks, and long-
term 6.3
±
0.6 months after symptom onset. In the RG, mean
plasma log BNP levels were significantly elevated in the acute
(RG vs NRG; 1.77
±
0.67 vs 1.29
±
0.53,
p
<
0.01) and early
phase (RG vs NRG; 2.31
±
0.54 vs 1.56
±
0.55,
p
<
0.01), and
long term (RG vs NRG; 2.07
±
0.55 vs 1.37
±
0.46,
p
<
0.01)
(Fig. 1).
Mean plasma BNP levels were significantly different between
the two groups (
p
<
0.01, repeated measures ANOVA) and
during each time phase (
p
<
0.01, repeated measures ANOVA).
Compared with the NRG, the RG mean plasma BNP levels were
prominently elevated in the early phase and long term. This
biphasic peak elevation of plasma BNP level was a characteristic
feature of the RG. As we examined plasma BNP measurements
throughout each study period, plasma BNP levels in the RG were
consistently higher than in the NRG.
Univariate regression analyses were conducted to determine a
surrogate marker for PMIR independent of other predictors. The
age, time from symptom to reperfusion, peak levels of troponin
I and CK-MB, LVEF and E/E
′
were significantly associated with
PMIR at the six-month follow up.
Hierarchical multiple regression analyses for optimal time of
PMIR were constructed (Table 4). In the multivariate model, after
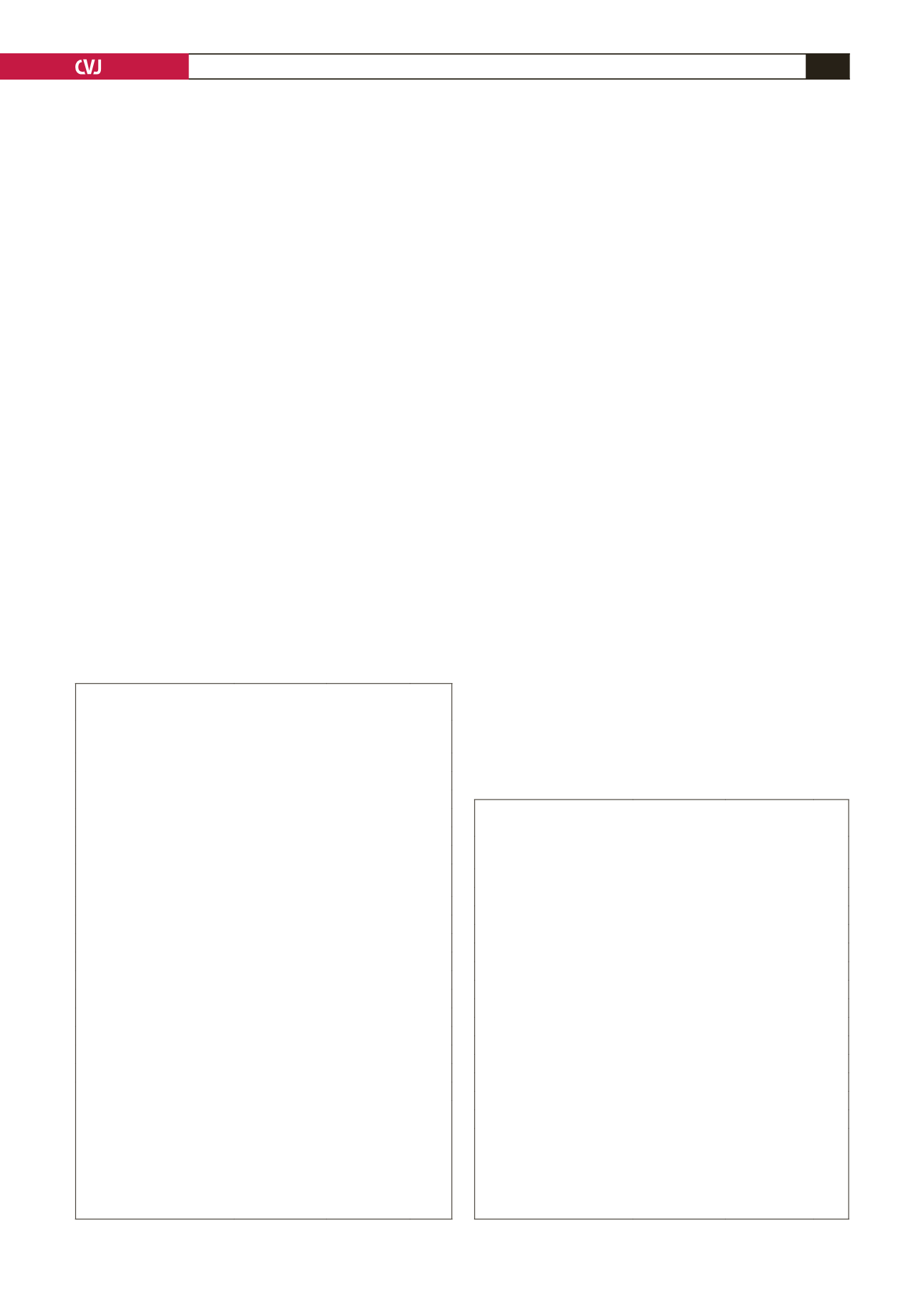
TABLE 1. BASELINE CLINICAL CHARACTERISTICS BETWEEN
NON-REMODELLINGAND REMODELLING GROUPS
Variable
Non-remodelling
group (
n
=
89)
Remodelling
group (
n
=
42)
p
Age (years)
58.1
±
11.1
63.1
±
11.9 0.02
Males,
n
(%)
68 (76.4)
26 (61.9)
0.14
Diabetes mellitus,
n
(%)
26 (29.2)
10 (23.8)
0.68
Hypertension,*
n
(%)
46 (51.7)
18 (42.9)
0.35
Current smoker,
n
(%)
49 (55.1)
23 (54.8)
0.47
Hypercholesterolaemia,
†
n
(%)
49 (55.1)
22 (52.4)
0.45
Time from symptom onset to
to reperfusion (h)
4.8
±
2.1
5.4
±
2.3
0.07
Killip class I,
n
(%)
41 (44.9)
17 (40.5)
0.26
NYHA class I,
n
(%)
70 (78.7)
24 (57.1)
0.03
Peak CK-MB (ng/ml)
170.9
±
109.9 246.8
±
88.1
<
0.01
Peak troponin I (ng/ml)
33.7
±
25.1
48.3
±
28.3
<
0.01
Discharge medications
Aspirin,
n
(%)
89 (100)
42 (100)
Clopidogrel,
n
(%)
89 (100)
42 (100)
β
-blockers,
n
(%)
81 (91.1)
36 (85.7)
0.22
ACEIs or ARBs,
n
(%)
85 (95.5)
38 (90.5)
0.49
Diuretics,
n
(%)
44 (49.4)
22 (52.4)
0.41
Statins,
n
(%)
86 (96.6)
40(97.6)
0.86
Data are mean
±
SD or numbers (percentage).
*Systolic pressure
>
140 mmHg and/or diastolic pressure
>
90 mmHg or
receiving antihypertensive drugs.
†
Total cholesterol
>
220 mg/dl and/or low-density lipoprotein cholesterol
>
130 mg/dl or receiving statin therapy.
NYHA, NewYork Heart Association; CK-MB, creatinine kinase myocar-
dial band; ACEI, angiotensin-converting enzyme inhibitor; ARB, angio-
tensin II receptor blocker.
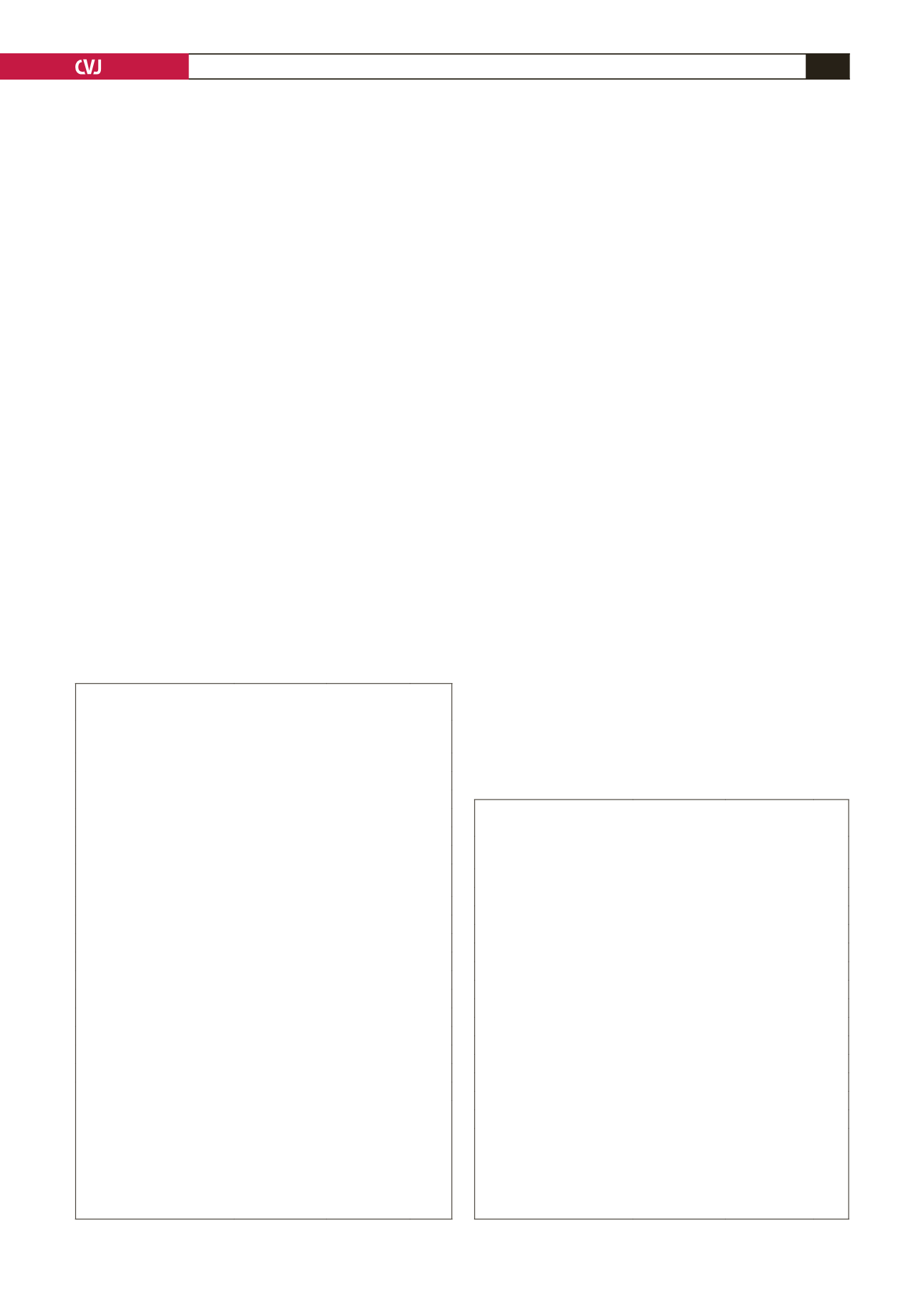
TABLE 2. BASELINE PROCEDURAL CHARACTERISTICS
BETWEEN NON-REMODELLINGAND REMODELLING GROUPS
Variable
Non-remodelling
group (
n
=
89)
Remodelling
group (
n
=
42)
p
Multi-vessel disease,
n
(%)
37 (41.6)
18 (42.9)
0.79
IRA
LAD,
n
(%)
38 (42.7)
26 (61.9)
0.04
LCX,
n
(%)
7 (7.9)
5 (11.9)
0.40
RCA,
n
(%)
44 (49.4)
11 (26.2)
0.01
Stent type (%)
DES,
n
(%)
81 (91.1)
38 (90.5)
0.72
BMS,
n
(%)
8 (8.9)
4 (9.5)
0.69
DES type (%)
SES,
n
(%)
29 (35.8)
16 (42.1)
0.43
PES,
n
(%)
39 (48.1)
18 (47.4)
0.47
ZES,
n
(%)
13 (16.1)
4 (10.5)
0.25
TIMI grade 3 after PCI,
n
(%)
84 (94.4)
36 (85.7)
0.09
Number of stents
1.25
±
0.53
1.27
±
0.36 0.33
Data are mean
±
SD or numbers (percentage).
IRA, infarct-related artery; LAD, left anterior descending artery; LCX,
left circumflex artery; RCA, right coronary artery; BMS, bare-metal
stent; DES, drug-eluting stent; SES, sirolimus-eluting stent; PES, pacli-
taxel-eluting stent; ZES, zotarolimus-eluting stent; TIMI, thrombolysis in
myocardial infarction; PCI, percutaneous coronary intervention.