CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 4, July/August 2014
e8
AFRICA
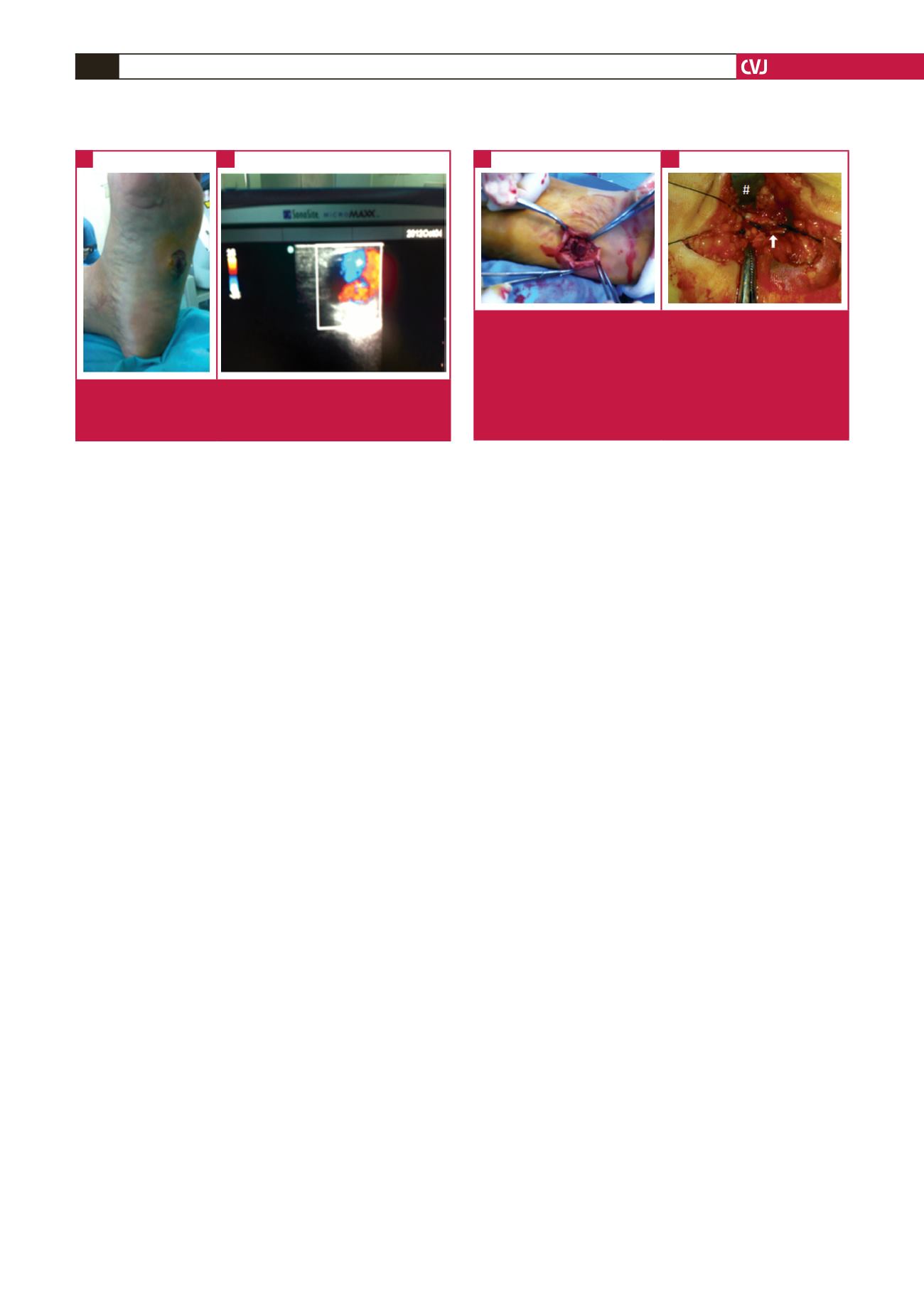
× 2.5 cm, was originating from the lateral plantar artery (LPA).
Colour duplex examination revealed turbulent flow within the
sac (Fig. 1B).
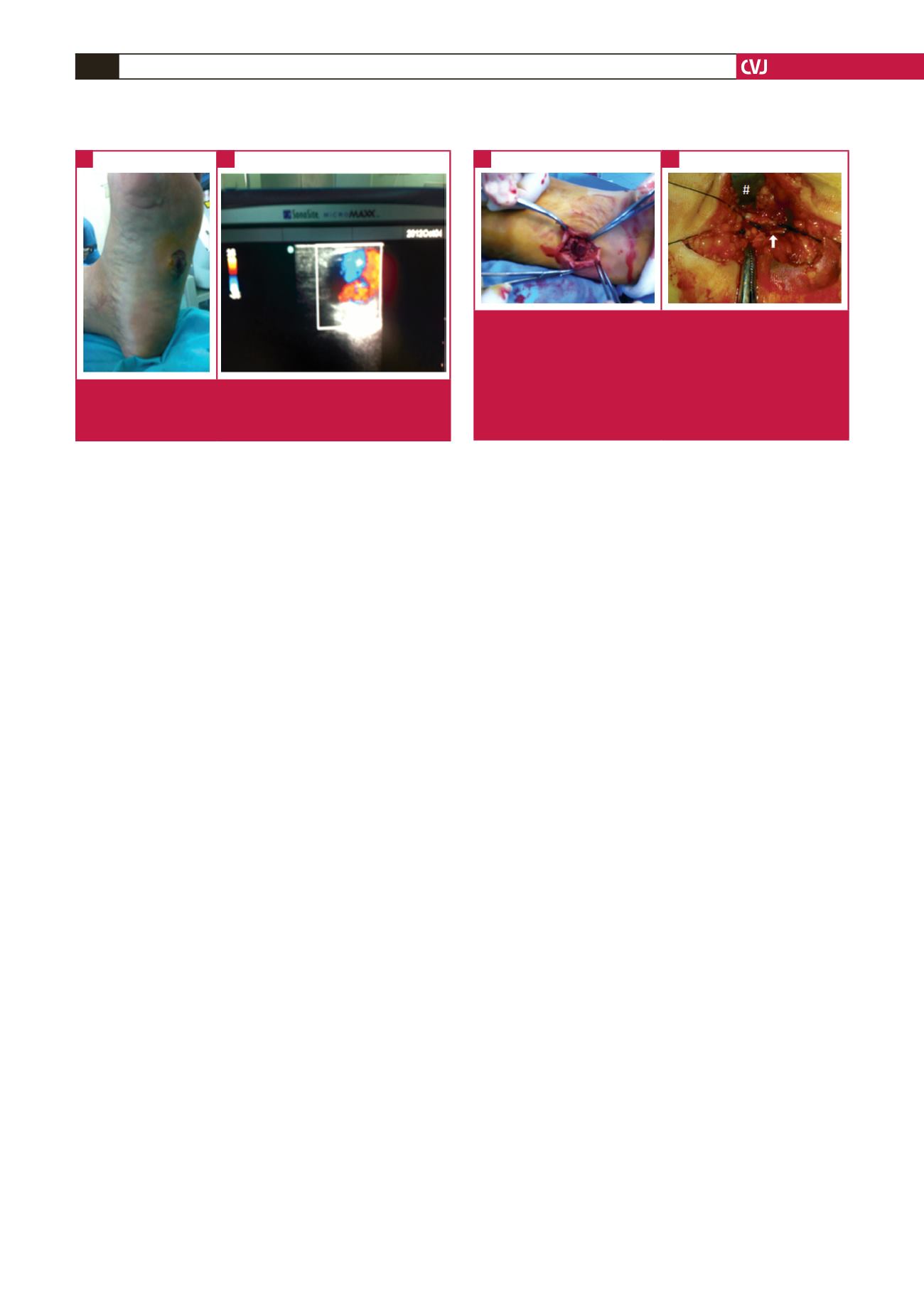
Under spinal anaesthesia, the aneurysmal sac was freed from
the surrounding tissues with blunt dissection until the plantar
fascia was exposed. To gain access to the plantar vasculature,
the plantar fascia was vertically incised and the flexor digitorum
muscle was retracted medially. After removal of the aneurysmal
sac, the injury of the LPA was detected and ligated proximally
and distally (Fig. 2).
Following the release of the tourniquet, no haemorrhage
at the surgical site was observed. Capillary filling of the toes
was normal. The hospitalisation period was uneventful and the
patient was discharged on postoperative day three.
Discussion
While significant bleeding at the time of injury was stated in
cases where the mechanism of injury was a cut from glass,
2,3,5
all cases with iatrogenic aetiology did not reveal significant
bleeding.
1,4
In comparison with stepping on a piece of glass, the
mechanism of injury in stepping on a construction nail, as in our
case, is quite different, in that the disruption of the tissues is less
than with glass laceration. Additionally, the penetration depth
of the nail cannot be predicted so significant bleeding would not
be obvious.
In our case, pain was persistent from the time of injury to
rupture. While pain is a non-specific symptom, persistence of it
was reported by Murakami
et al
.
3
In our opinion, persistence of
pain should indicate pseudo-aneurysm or abscess formation. At
that point, a simple physical examination looking for pulsatility
is essential. While it may be impossible to evaluate all plantar
injury cases with duplex ultrasonography, it can provide salient
data and accurate evaluation.
The time interval from injury to diagnosis ranges from 10
days to eight weeks.
1-5
In our opinion, this time gap depends on
the symptomatology of the case and/or the paucity of follow up.
A pulsatile mass, which was stated to be the presenting symptom
in three cases,
4,5
is the cornerstone of diagnosis of pseudo-
aneurysm.
In our case rupture occurred in the third week after injury,
as in another case.
2
Thornton
et al
. stated that continuous
and intermittent trauma of the plantar region can lead to
expansion and rupture of the pseudo-aneurysm.
5
In addition
to this, ambulation, resulting in compression of the plantar
region, could lead to different time intervals for formation of
the pseudo-aneurysm and for it to become symptomatic or
physically evident. This also makes it difficult to decide how long
the follow up of these cases should be.
The anatomy of the plantar vasculature was studied in
cadaveric dissections and, when compared with the medial
plantar artery (MPA), the course of the LPA is more superficial,
and the MPA is protected by the musculature. As a consequence,
the LPA is more vulnerable to injury.
5
Other than being more
superficial than the MPA, the LPA coincides with the footprint,
which is the weight-bearing plantar region and the first to touch
the ground during ambulation. Therefore the LPA is more
vulnerable to injury.
Conclusion
In cases of plantar injury, significant bleeding at the time of
injury depends on the mechanism of injury. Prompt surgical
exploration in cases of bleeding and in cases with injury
extending beyond the plantar fascia appears to be beneficial.
Deciding on the duration of follow up in cases without evident
bleeding is a challenge and duplex ultrasonographic evaluation
in selected cases may be beneficial. Moreover, a prospective
study including larger volumes of cases with plantar injury is
needed with regard to symptomatology, influencing factors that
contribute to pseudo-aneurysm formation, and differences in
time interval for the pseudo-aneurysm to become symptomatic.
I thank my colleagues for supporting me in writing this article. This article
was presented as a poster presentation (HPP-239) at the 9th International
Congress of Update in Cardiology and Cardiovascular Surgery which was
held between 21 and 24 March 2013 in Antalya, Turkey.
References
1.
Baeza L, Farrell ED, Salgado CJ. Medial plantar artery pseudo-
aneurysm following percutaneous pinning for Lisfranc fracture-disloca-
tion.
J Am Podiatr Med Assoc
2009;
99
(1): 58–60.
2.
Economou P, Paton R, Galasko CS. Traumatic pseudoaneurysm of the
Fig. 1.
View of the pseudo-aneurysm on the left sole (A).
Ultrasonographic evaluation revealed a pulsatile aneu-
rysmal sac with turbulent flow (B).
A
B
Fig. 2.
Intra-operative view of the case. (A) The aneurysmal
sac was reached under the plantar fascia. (B) The
flexor digitorum muscle was retracted medially (#).
After excision of the aneurysmal sac, the injury of the
LPA was detected. Ligation of the LPA proximally and
distally of the injury was performed. Note the arrow
indicates lateral plantar nerve.
A
B