CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 4, July/August 2014
AFRICA
e11
artery banding would be a palliative intervention and the
probable survival outcome was not expected to change. The
family insisted on the surgical procedure, and according to the
local medical laws, the patient was scheduled for surgery.
The baby was accepted for anaesthesia as class ASA IV. The
parents were informed about the risks and a written consent was
obtained. Initial laboratory investigations showed abnormalities
such as aspartate aminotransferase (AST) 86 μg/l, indirect
bilirubin 7.7 mg/dl, potassium 6.0 meq/l, albumin 2.4 g/dl, and
platelet 55 000 per mcl. Pre-operative laboratory investigation
was normal.
No premedication was given, and the baby was transferred
to the operating room with oxygen supply in the transport
incubator. After the application of standard non-invasive
monitoring, including ECG, SpO
2
and NIBP, due to the problem
of existing vascular access, general anaesthesia was induced with
sevoflurane 8% in 50:50% oxygen in air. We refrained from using
a high concentration of oxygen due to the risk of retinopathy of
prematurity.
Peripheral venous access was achieved with a 24-G iv
catheter at the dorsum of the left hand. In order to facilitate
endotracheal intubation, 2 mcg/kg of fentanyl and 0.5 mg/kg of
rocuronium bromide were given intravenously. After two minutes
of ventilation with 100% O
2
via a face mask, a laryngoscopy was
performed using a size 0 Miller blade. Laryngoscopy revealed
grade II Cormach-Lahane, and intubation was achieved easily
with a 3.0 mm uncuffed endotracheal tube.
Central venous and arterial accesses were achieved via the
right femoral route with 4-F double-lumen 5-cm and 22-G single-
lumen 5-cm catheters, respectively. Anaesthesia was maintained
using controlled ventilation with sevoflurane 1.5–2% in 50:50%
oxygen in air; 1 mcg/kg of fentanyl and 0.2 mg/kg of rocuronium
were added as needed. Pre-banding invasive blood pressure,
which was 66/34 (45) mmHg, increased to 84/48 (60) mmHg
following PDA ligation and banding. Also SpO
2
decreased from
99 to 95% after banding (FiO
2
=
0.5).
The operation lasted for 35 minutes without any surgical and/
or anaesthetic problems. After pulmonary banding, 5 mcg/kg/
min dopamine infusion was started for haemodynamic support.
After an uneventful closure of the PDA and pulmonary artery
banding, the baby was transferred to the NICU intubated with
mechanical ventilation support. The baby was extubated on the
second day postoperatively. She died in the NICU 10 weeks
later after an episode of resistant bradycardia despite proper
resuscitation.
Discussion
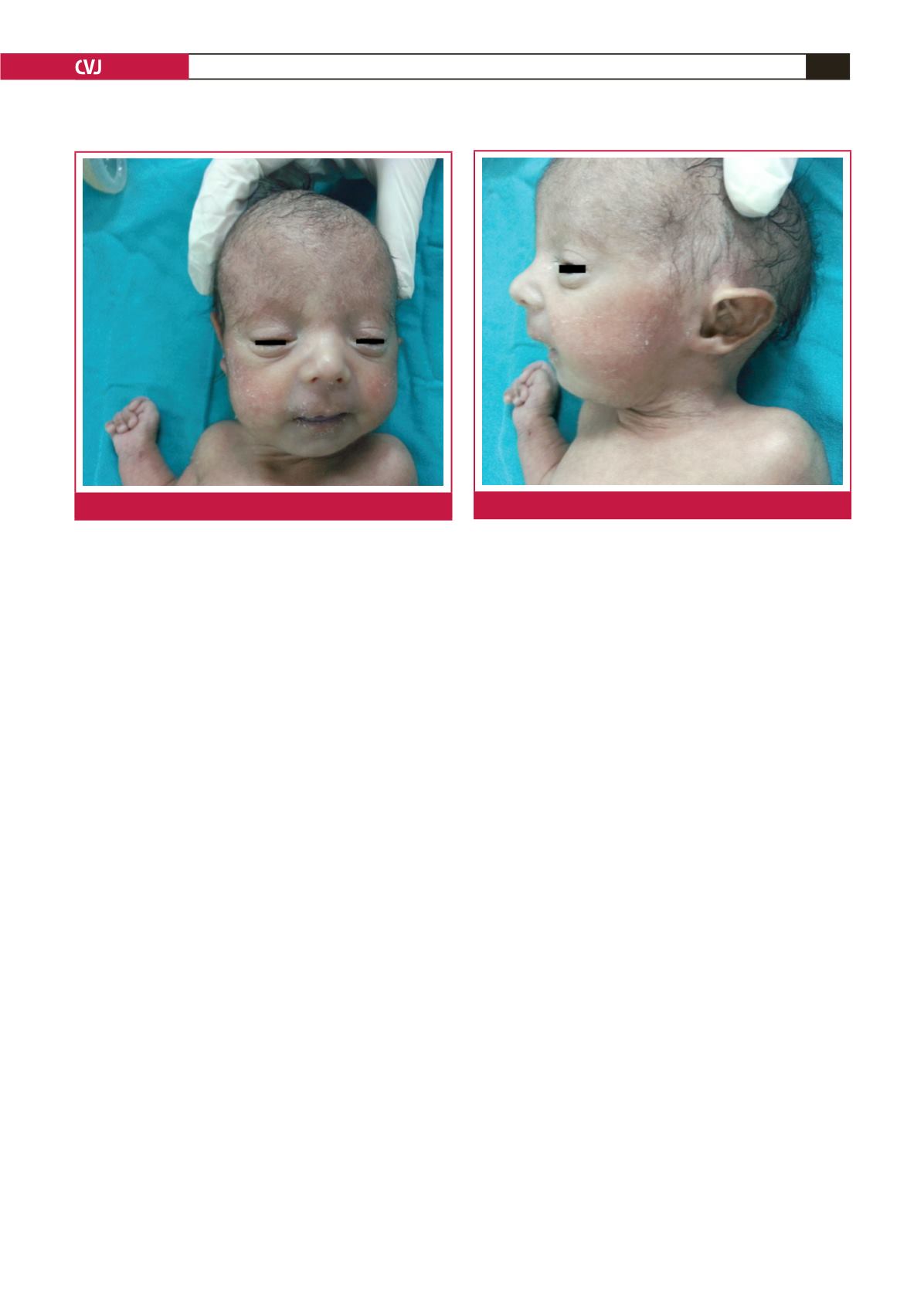
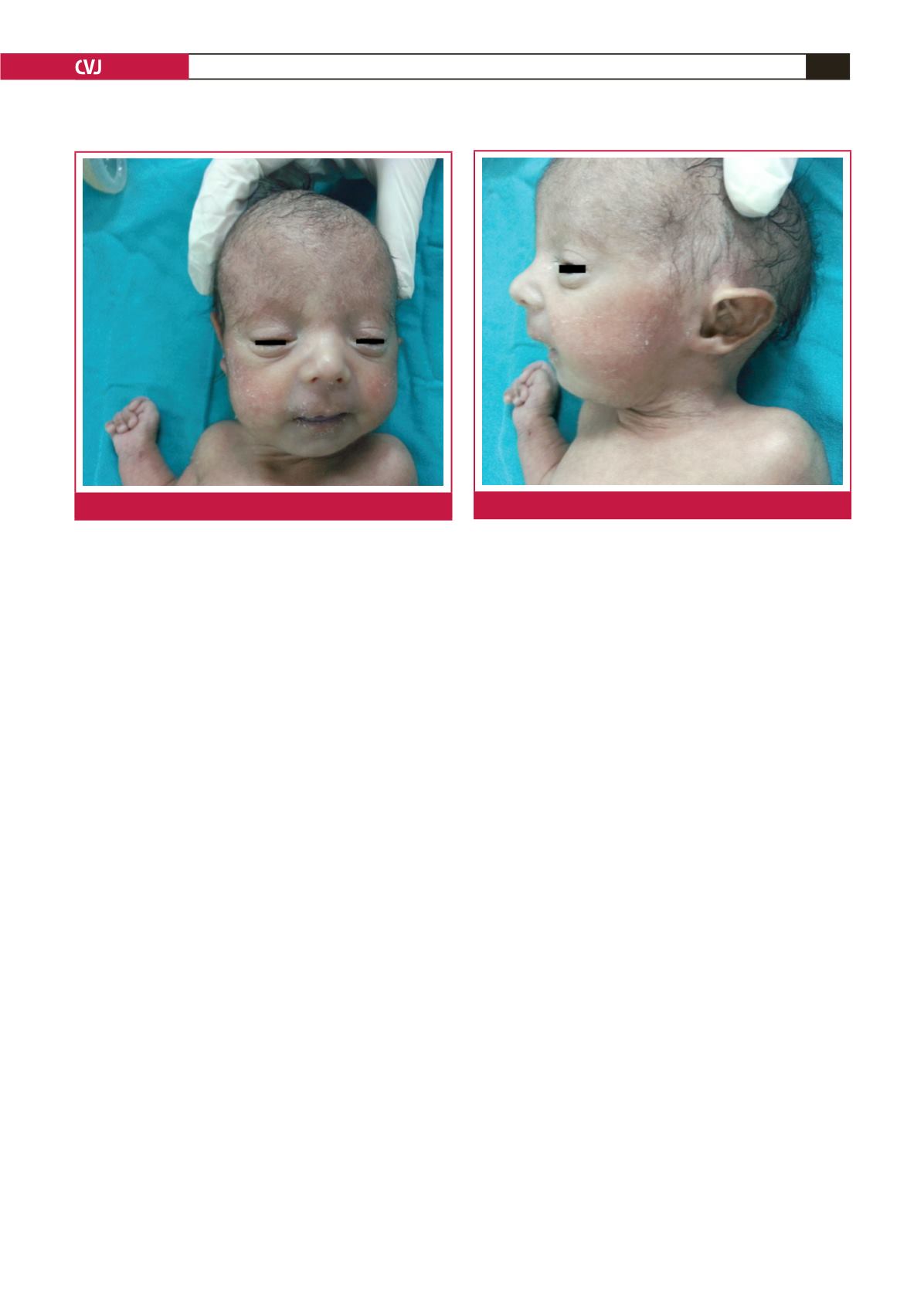
The clinical pattern of trisomy 18 is characterised by growth
deficiency that starts in the prenatal period; specific craniofacial
features such as dolichocephaly, short palpebral fissures,
micrognathia, external anomalies of the ears, and redundant
skin at the back of the neck; and marked psychomotor and
cognitive developmental delay. The presence of major systemic
malformations is common, and any organ and system can be
affected.
Prenatal and early postnatal infant mortality rates are high
when compared to the general population.
4
The postnatal
median survival of children with trisomy 18 is three to 4.5 days;
approximately 50% of babies with trisomy 18 live longer than
one week and only five to 10% of children survive beyond the
first year. One of the major causes of death is cardiac failure due
to congenital heart defect-related problems.
5
The severity of the cardiac and extra-cardiac lesions is
an important factor for the timing and extent of cardiac
surgery. Kaneko
et al
. hypothesised that trisomy 18 patients who
underwent intra-cardiac repair had more complicated cardiac
lesions and, therefore, mortality rates were increased.
6
We believe
similarly that postponement or abandonment of the cardiac
operation can have a negative impact on survival because of
longer exposure to excessive pulmonary blood flow and heart
failure. Therefore palliative cardiac surgery may be sufficient to
relieve symptoms, prevent heart-related death, and improve life
expectancy when performed at an early stage.
Due to the limited data regarding anaesthesia techniques
in patients with trisomy 18, it is impossible to suggest a
Fig. 1.
Dysmorphic face of the baby.
Fig. 2.
Malformed ear of the baby.