
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
AFRICA
85
Peripartum cardiomyopathy (PPCM)
PPCM is a potentially life-threatening heart disease emerging
towards the end of pregnancy or in the first months postpartum
in previously healthy women.
6
In most patients, cardiac function
recovers, however, the mortality rate is up to 5–32%, and
many patients develop chronic heart failure.
7
In the acute
phase, PPCM manifests as acute heart failure (AHF) and the
diagnosis relies on exclusion of other causes of AHF. A novel
finding is the discovery that oxidative stress-mediated cleavage
of the nursing hormone prolactin into a smaller biologically
active sub-fragment (16-kDA prolactin) may be a major factor
initiating and driving PPCM.
Treatment recommendations rely on standard acute heart-
failure therapy. After the acute phase, in addition to the standard
treatment of chronic heart failure, novel disease-specific strategies,
such as bromocriptine, should be considered. PPCM in itself is
a prothrombotic condition and embolic events leading to strokes
are common. Therefore, all patients with an ejection fraction
(EF)
<
35%, those receiving bromocriptine, and particularly if
a thrombus has been visualised on echocardiography, should
be anticoagulated with intravenous heparin or low-molecular
weight heparin antepartum, and receive warfarin after delivery.
Ischaemic heart disease during pregnancy
The incidence of fatal ischaemic heart disease (IHD) in pregnancy
ranges between 0.48 and 0.76 per 100 000 pregnancies. The most
common presenting symptom in pregnancy is chest pain, which
is present in 95% of women with IHD.
8
In a systematic review of
IHD in pregnancy, 93% of women who had an acute myocardial
infarct (AMI) due to atherosclerosis had risk factors, compared
with AMI caused by coronary dissection (43% had risk factors)
and thrombus or emboli (68% had risk factors).
8
Therefore
lifestyle factors such as obesity and smoking are important risk
factors in pregnancy.
Coronary artery dissection and thromboembolic coronary
events are the most common causes of IHD reported in
pregnancy.
8
Diagnosis in pregnancy is based onECG (ST-segment
deviation will be seen in about 89% of cases) and laboratory
investigations. In the United Kingdom sub-standard care due
to delayed diagnosis occurred in 46% of cases of maternal
death. Therefore, a high index of suspicion is needed for IHD in
pregnant women who present with chest pain and risk factors.
Aortic dissection
In the same United Kingdom registry for the 2006–2008
triennium there were seven maternal deaths due to aortic
dissection. In most cases, patients presented with severe chest or
interscapular pain requiring opiate analgesia, and the diagnosis
was delayed as appropriate investigations were not performed.
Hormonal changes and increased haemodynamic stress
predisposes to aortic dissection in pregnancy, but the exact
mechanism is unclear.
9
Obesity, multiparity, raised systolic
blood pressure, heart conditions and pre-existing connective
tissue disorders such as Marfan and Turner syndrome, Ehlers–
Danlos type IV, coarctation of the aorta and bicuspid aortic
valve increase the risk for aortic dissection. This diagnosis must
be considered in the differential diagnosis of pregnant women
who present with chest pain, particularly in the presence of
systolic hypertension. Appropriate imaging includes computed
tomography chest scan, magnetic resonance imaging, as well as
transthoracic or transoesophageal echocardiogram.
Cardiac disease and maternity in the
developing world
Heart disease is a common problem in pregnancy in LMICs;
10
it increases the risk of morbi-mortality in these women and,
as in HICs, seems to be the leading non-obstetric cause of
maternal death. Similarly to the situation in HICs, risk factors
such as hypertension and diabetes are contributors to maternal
morbidity and mortality in LMICs, owing to their prevalence
in the general population.
11-16
However, a unique disease profile
is found in LMICs due to the existence of poverty-related
cardiovascular diseases.
Risk factors such as hypertension, obesity and diabetes
are increasingly important, occuring in high numbers in
some countries, urban settings and specific sub-populations
in sub-Saharan Africa, Asia and Latin America. In Africa,
hypertension is most frequently observed in both rural and
urban communities, with prevalence rates in young populations
ranging from 9.3 to 48.1%.
11,12
Smaller variations were found in
India, where the overall prevalence for hypertension was 29.8%
(95% confidence interval; range 26.7–33.0%) and significant
differences were noted between rural and urban areas.
13
A meta-
analysis of published studies on the prevalence of hypertension
in Chinese cities found an average of 21.5%,
14
while in Iran
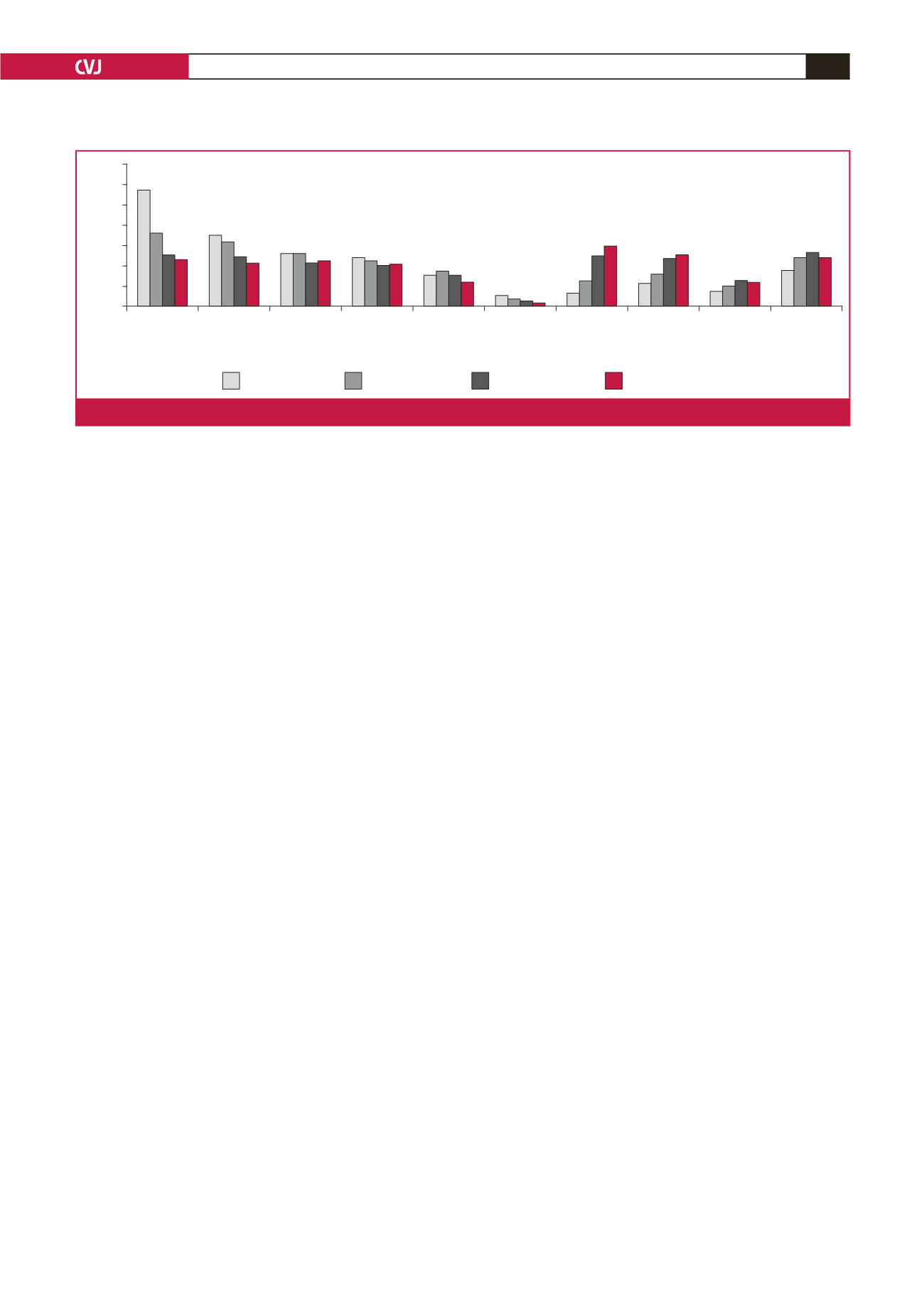
Haemorrhage Hypertensive
disorder
Infection Thrombotic
pulmonary
embolism
Amniotic
fluid
embolism
Anaesthesia Cardio-
vascular
condition
Cardio-
myopathy
Cerebro-
vascular
accident
Other
medical
condition
35
30
25
20
15
10
5
0
Percentage of deaths
1987–1990
1991–1997
1998–2005
2006–2009
Fig. 1.
Causes of pregnancy-related mortality in the United States, 1987–2009 (from Creanga
et al
., 2014
2
).

















