
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
AFRICA
87
Socio-demographic and health systems issues
In LMICs, delays in enrolment for antenatal care and lack of
adequate healthcare hamper the recognition of life-threatening
conditions and the control of preventable factors that lead
to cardiac decompensation during pregnancy. Low capacity
for diagnosis at peripheral levels of the health systems and
lack of awareness of the risks related to pregnancy result in
few pregnant women being identified as having heart disease,
therefore determining inadequate management and considerable
impact on maternal and foetal outcome. On the other hand,
acute and chronic complications and common endemic diseases
may also further contribute to increase the risk of pregnant
women dying during pregnancy, such as the case with cardiac
tuberculosis, schistomosmiasis and syphilis.
33
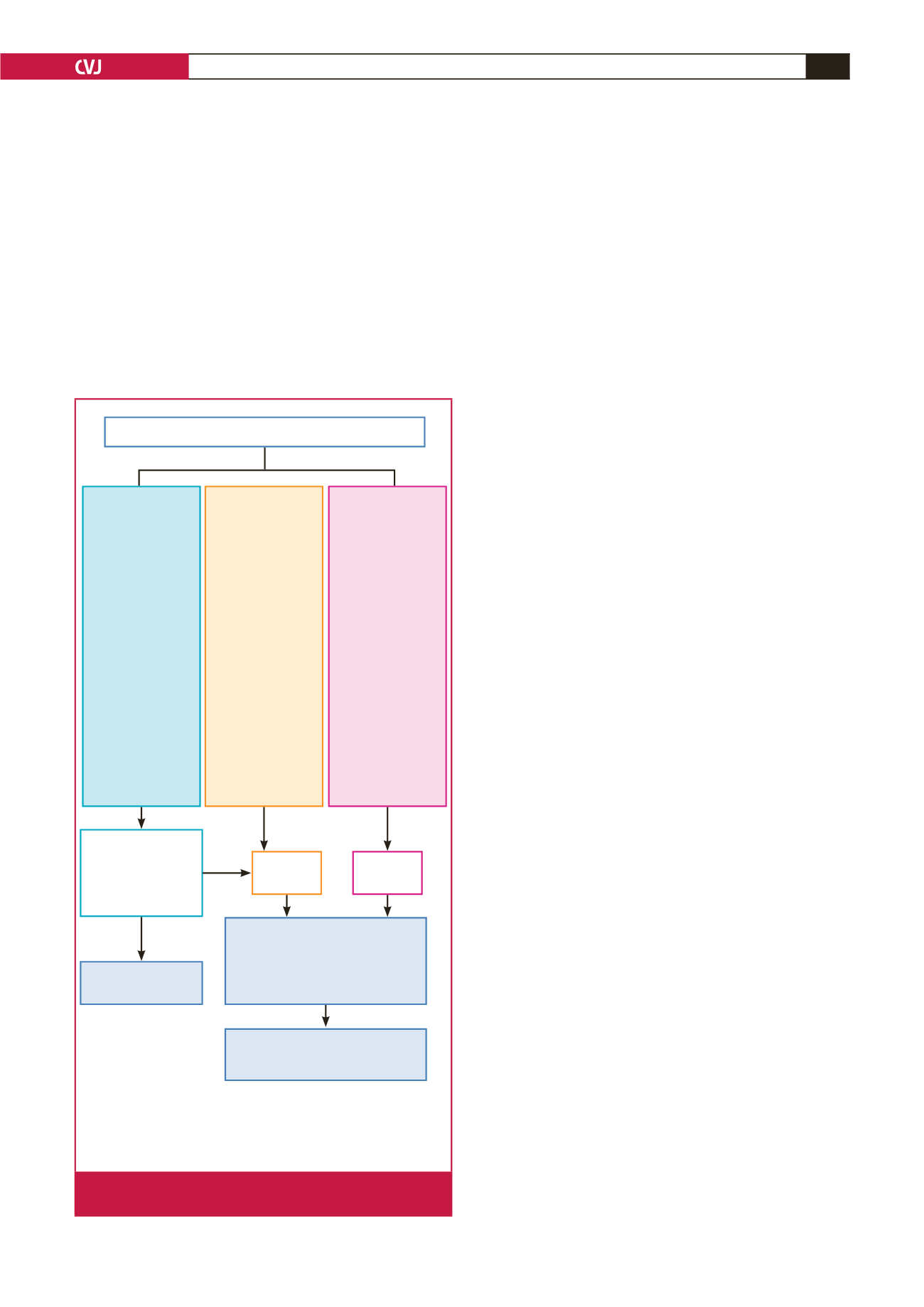
For the identification and management of pregnant patients
with cardiovascular disease, we would therefore recommend
that (1) all pregnant women should be screened at booking
for underlying medical or surgical conditions; (2) women with
known or recently detected cardiovascular disease should
undergo risk assessement based on an algorithm (Fig. 2); (3)
women presenting with difficulty in breathing, systolic blood
pressure of
<
100 mmHg, heart rate
>
120 beats per minute or
appearing cyanotic, need to be transferred by ambulance to a
tertiary centre within 24 hours; those presenting with signs of
fluid overload should receive a bolus of lasix 40 mg IV and
oxygen per face mask prior to transfer; (4) clinicians should have
a low threshold for investigating pregnant or recently delivered
women (up to six months postpartum), especially those with
cardiovascular risk factors (hypertension, diabetes), suspected
rheumatic heart disease or with symptoms such as shortness of
breath or chest pain; appropriate investigations include ECG,
chest X-ray, echocardiogram and CT pulmonary angiography;
(5) certain patients with high-risk cardiovascular disease may
need careful monitoring for up to one year postpartum due to
the high risk of developing heart failure, serious arrhythmia and
embolic events.
Socio-economic and demographic factors such as persistently
high fertility rates, social pressure to conceive, insufficient access
to contraceptive methods, as well as social or familial ostracism
towards women who use contraception, may further contribute
to increasing the risk of death due to cardiac disease, even in
women who have been diagnosed.
34
Conclusions
Available data on maternal mortality rates reveal the
pre-imminence of cardiovascular disease as the most important
medical cause of non-obstetric maternal death in both developed
and developing countries. Failure to systematically search for
cardiac disease in pregnant women has led to late diagnosis and
high rates of fatal complications. Therefore active screening
for cardiac disease in pregnant women is warranted, if the
millennium development goal of reducing the maternal mortality
ratio is to be achieved.
In LMICs algorithms for cardiac screening of pregnant
women should consider the unique profile of cardiovascular
disease, including rheumatic heart disease, cardiomyopathies,
HIV/AIDS, haemoglobinopathies and undetected/untreated
congenital heart defects. Such active strategies for suspected
and previously known cardiac disease in pregnancy are expected
to prevent a substantial proportion of maternal morbidity and
mortality.
References
1.
The Millennium Developent Goals Report 2013.United Nations, 2013;
UNDP, UNFPA; UNICEF; UN Women; WHO.
2.
Creanga AA, Berg CJ, KO JY,
et al
. Maternal mortality and morbidity in
the United States: Where are we now?
J Women’s Health
2014;
23
: 3–9.
3.
Nelson-Piercy C. The UK maternal death report.
Obstet Med
2015;
8
: 3.
4.
Nelson-Piercy C. Cardiac disease in Centre for Maternal and Child
Enquiries (CMACE).
Br J Obstet Gynecol
2011;
118
(suppl. 1); 109–115.
Primary and secondary care maternal facility
Modified WHO
classification I
• Previously diag-
nosed hyperten-
sion, diabetes,
morbid obesity
(BMI > 35 kg/m
2
)
• Successfully
repaired simple
lesions
• Uncomplicated,
small or mild mitral
valve prolapse,
pulmonary stenosis
• Palpitations – no
dizziness
Modified WHO
classification
III–IV
• Mechanical valve
and symptoms
• Complex congenital
or cyanotic heart
disease
• Pulmonary hyper-
tension any cause
• Previously diag-
nosed peripartum
cardiomyopathy
• Severe ventricular
impairment (EF <
45%, NYHA FC > II)
• Severe mitral
stenosis and aortic
stenosis
• Aortic dilataion
> 45 mm (bicuspid
AV, Marfan)
Modified WHO
classification II
• Unoperated ASD
and VSD
• Repaired tetralogy
of Fallot and coarc-
tation
• Arrythmias and
dizziness
• Mild left ventricular
impairment (EF >
45%, NYHA FC II)
due to newly diag-
nosed PPCM or HT
heart failure
• Previously diag-
nosed RHD with
murmurs and/or
recently assessed
asymptomatic
mechanical valve
Tertiary care
maternal facility
Tests: BP, ECG,
echocardiogram and
assess for murmurs
Non-urgent
referral
Urgent
referral
Joint cardiac–obstetric–
anaesthetic CDM team
Consulting with paediatric cardiologist,
endocrinologist, radiologist, HIV
specialist and others
Follow up with
maternity service
Postpartum referral to main cardiac
clinic, if indicated, for management
and possible cardiothoracic surgery
Abnormal
Normal
BMI: body mass index; ECG: electrocardiogram; ASD: atrial septal defect;
VSD: ventricular septal defect; EF: ejection fraction; NYHA FC: New York
Heart Association functional class; PPCM: peripartum cardiomyopathy;
HT: hypertension; AV: aortic valve
Fig. 2.
Referral algorithm for suspected and previously known
cardiovascular disease in maternity.

















