
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
80
AFRICA
service-delivery mechanisms within existing programmes.
Innovative programmes have to be explored to highlight PCC.
Consequently, adequate financial resources should be mobilised
to support strategic implementation, monitoring and evaluation
of viable PCC programmes.
2
Having outlined the vision for PPC and the specific need
within the African continent, we will focus our attention on some
specific conditions requiring comprehensive PPC and assessment.
Given the burden of disease of congenital, rheumatic and
hypertensive heart disease, as well as HIV/AIDS, we will discuss
these conditions by suggesting clear guidelines for clinicians
caring for such patients, as well as strategies to improve outcomes
relating to these conditions. Although we describe specific medical
interventions to optimise health prior to pregnancy, the general
evidence-based interventions should be the platform upon which
these are based. These include screening for anaemia, nutritional
supplementation (iron and folate), information, education and
counselling, food supplementation, promoting exercise and a
healthy diet, and family planning and child spacing (Table 2).
Systematic review
We performed a literature review of publications in PubMed,
employing no language restriction, on the use of pre-conception
counselling in Africa. Search terms included combinations
of ‘((preconceptual[All Fields] AND (‘counselling’[All Fields]
OR ‘counseling’[MeSH Terms] OR ‘counseling’[All Fields])))’
and ‘Africa OR sub-Saharan Africa’ or Afric*. We identified
no previous studies that report pre-conception counselling in
Africans.
This review responds to the need for pre-conception
counselling in African women. It provides an overview of the
need, details and goals of such counselling and then describes
specific important conditions.
There are several studies detailing pre-conception counselling
in different situations similar to the ones described. However,
these are all from developed countries, therefore the findings
cannot be generalised to the African context.
Our review highlights the need for multidisciplinary team
approaches to pregnancy and for pre-conception clinics in
specific key disease groups. We anticipate that this review will
be an important resource for physicians, obstetricians and
gynaecologists working in developing country settings.
Congenital heart disease
The story of congenital heart disease is one of the major
successes of medicine in the last 50 years. The vast majority of
lesions are amenable to surgery and neonatal surgery is now the
norm rather than the exception.
7
Many women with congenital
heart disease are currently in their childbearing years, and
desire pregnancy to bear their own children; however, there is a
startling difference in the situation in Africa.
8
With very few specialised cardiothoracic centres in Africa,
the majority of children requiring congenital heart surgery have
no access to these centres.
9
Adults with congenital heart disease
in Africa fall into two categories, namely, those who are ‘post-
operation’ or ‘post-intervention’, and adults with ‘previously
undiagnosed’ congenital heart disease (recognised for the first
time at pregnancy, or in early adulthood). The latter category
is seldom encountered in the developed world. Both categories
of women should be offered comprehensive PPC by a dedicated
multidisciplinary team, because each category presents a unique
set of cardiac and obstetric challenges, requiring an individualised
assessment of risks and a carefully documented care plan.
10
A large proportion of women attending cardio-obstetric
clinics have documented congenital heart disease. A recent
review of one clinic in Cape Town, South Africa, showed that
almost a third (32%, 15 with previous operations) had congenital
heart disease.
11
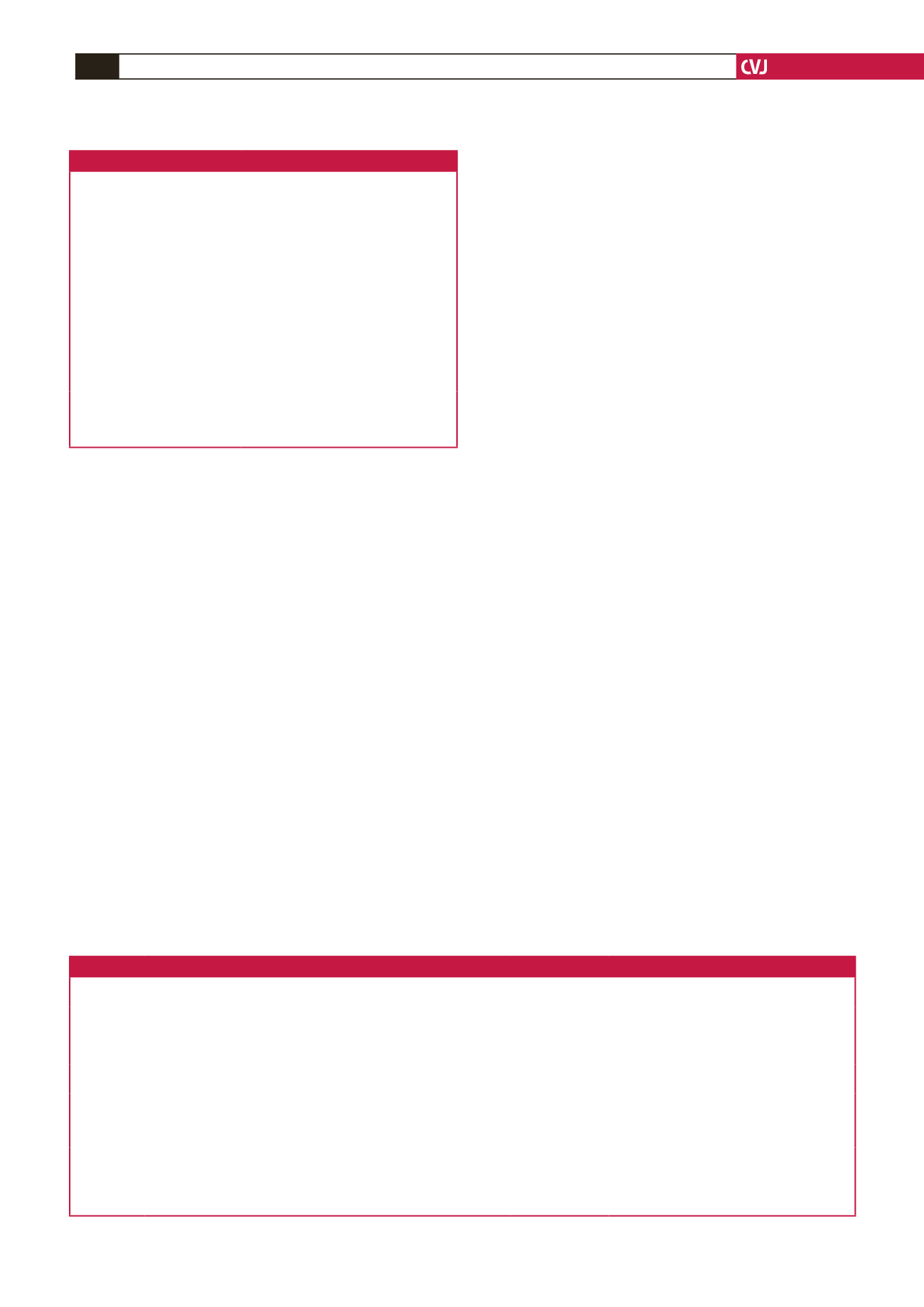
Table 1. Pre-conception care
WHO package of
evidenced-based interventions
Components of
pre-conception
care
Specific conditions
addressed by pre-conception
care only
• Nutritional conditions
• Genetic conditions
• Vaccine-preventable conditions
• Environmental health
• Infertility/subfertility
• Female genital mutilation
• Too early, unwanted and rapid
successive pregnancies
• Sexually transmitted infections
• HIV
• Interpersonal violence
• Mental health
• Psychoactive substance use
• Tobacco use
• Medical
history
• Psychosocial
issues
• Physical
examination
• Laboratory
tests
• Family
history
• Nutritional
assessment
• Conditions that need
time to correct prior to
conception
• Interventions not usually
undertaken in pregnancy
• Intervention considered
only because a pregnancy
is planned.
• Conditions that might
change the choice/timing
or method to conceive
• Conditions requiring early
post-conception pre-natal
care
Adapted from: Preconception care to reduce maternal and childhood mortality
and morbidity. Meeting report and packages of interventions: WHO HQ, Febru-
ary 2012; Preconception care: Greater New York Chapter of the March of Dimes
Preconception Care Curriculum Working Group 2015.
Table 2. Clinical pearls: planning pregnancy with certain medical conditions
Medical
condition
Preventative measures and supplementation
Contra-indications
to pregnancy
Key points
Congenital
heart disease
Rubella vaccination
WHO IV risk score Needs comprehensive risk assessment before preg-
nancy
Rheumatic
heart disease
Primary prevention of group A streptococcus with penicillin
Institute secondary prevention with penicillin after a diagnosis of ARF/RHD
WHO IV risk score Needs comprehensive risk assessment before preg-
nancy
Hypertension Identify and treat secondary causes, treat sleep-disordered breathing, lifestyle
changes
ACE inhibitors and
ARBs
Normalise pre-pregnancy blood pressure
HIV
Treat co-morbidities
None
Avoid efavirenz if possible
Optimise ART to maximal suppression of viral load
Improved ART adherence
Advise appropriate contraception
General
Screen for anaemia
Food supplementation, iron and folate supplementation
As per examination Information, education and counselling
Promote exercise and healthy diet
Family planning and spacing
Weight control
Substance and tobacco control

















