
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
AFRICA
121
such as CRP, tumour necrosis factor-
α
(TNF-
α
) and IL-6 have
been associated with an increased risk for CVD.
33
Vaccarino
and colleagues investigated depression, inflammation and
cardiovascular outcomes of women.
33
Women with established
depression had 70% higher CRP levels than women without
depression.
33
The study also suggested that the association between
depression and CVD cannot be explained by inflammation
alone.
33
Kamarck and colleagues performed a prospective study
to determine the directionality of the association between
depression and inflammatory markers in both men and women.
1
The study found that only BMI had a greater association with
increased CRP and IL-6 than depression.
1
Depression during pregnancy and postnatal
depression
Perinatal depression is a serious and prevalent mental health
condition occurring towards the end of pregnancy and up until
the first year postpartum.
34,35
Depression is disabling for women
and is most common during the childbearing years.
35
Postpartum
depression refers to the depressive disorders occurring during the
postpartum period, up until the first year following childbirth.
35
In developed countries, studies have shown that the prevalence
of postpartum depression is around 10–15%.
36
However, in
developing regions, the proportion is often double that of
developed regions. A study in western Nigeria reported the
incidence of perinatal depression during pregnancy to be 31.3%.
37
A South African study found that 32% of the perinatal
women screened for maternal depression qualified for referral to
counselling.
5
The case study found that there is a deficiency in
screening for depression in primary healthcare in South Africa
and many cases are not identified.
5
They used the Edinburgh
Postnatal Depression Scale (EDPS) as a screening tool.
5
This is a
validated 10-item questionnaire used for screening for a probable
diagnosis of depression, both pre- and postpartum.
6,36
A separate study performed in peri-urban settlements in Cape
Town, South Africa, investigated the prevalence of depressed
mood during pregnancy in these populations.
6
The study found
that 39% of the pregnant women showed signs of depression.
The psychosocial risk factors for maternal and postpartum
depression include past history of mental illness, mental
disturbance during pregnancy, family history of depression, low
socio-economic status and poor interpersonal relationships.
38
Postnatal depression is sometimes preluded by depression during
pregnancy.
7
Depression as a potential risk factor for CVD
during peripartum
Depression has been confirmed to be a risk factor for CVD in
general.
30
The mechanism by which depression is thought to
contribute to the development of CVD is through an increase
in oxidative stress, as well as inflammation.
33
Oxidative stress
and inflammation have both been suggested to contribute to
the development of PPCM and pre-eclampsia.
26,29
Depression
during pregnancy may contribute to hypertension via excretion
of vasoactive hormones.
39
A prospective population study
suggested that depression in early pregnancy was a risk factor for
pre-eclampsia later in pregnancy.
39
Depression has been linked to
a higher risk of heart failure as well as poorer outcomes.
40
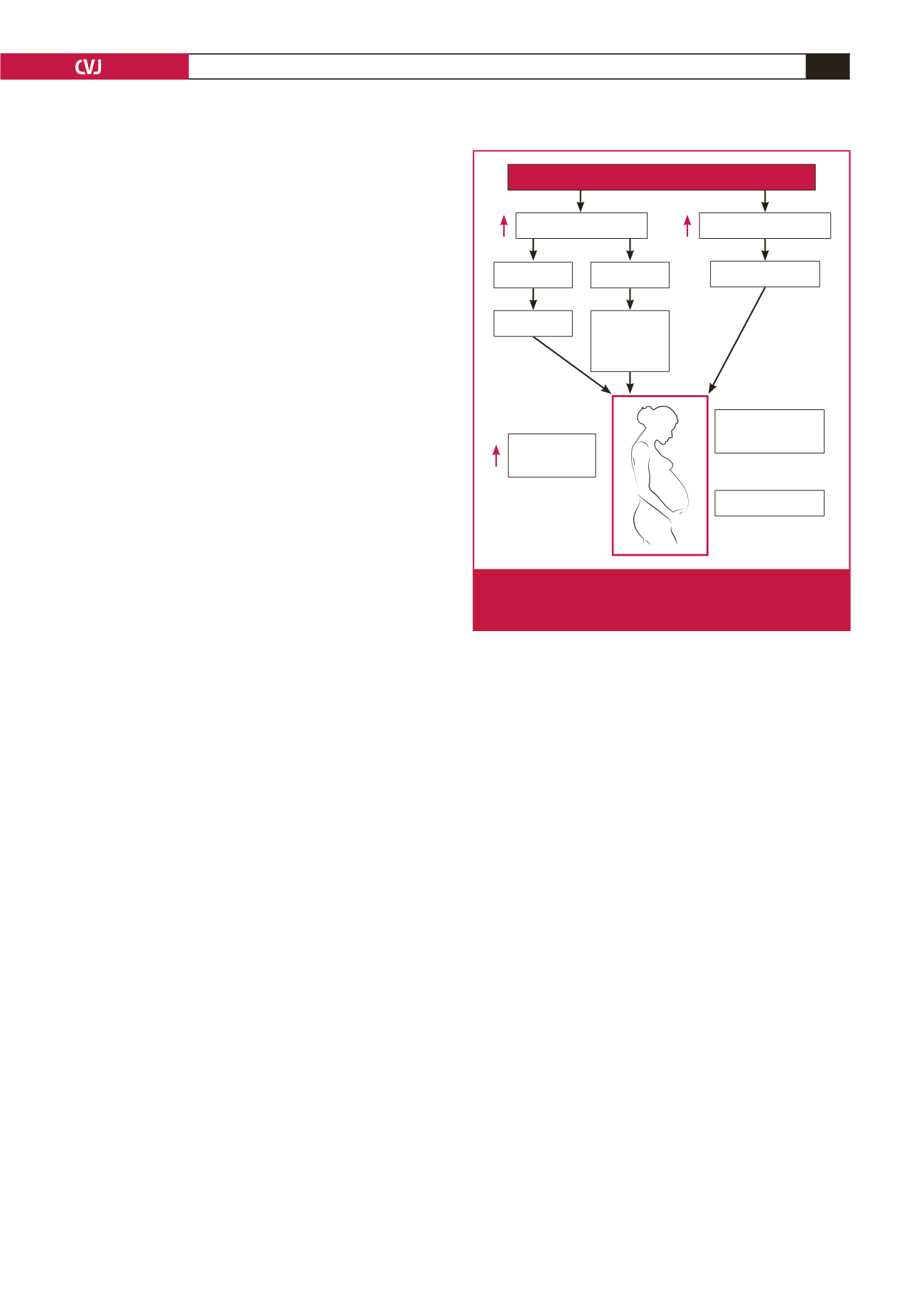
A hypothetical mechanism by which depression during
pregnancy and postpartum may contribute to the development
of PPCM and pre-eclampsia is shown in Fig. 2. The pathological
increase in oxidative stress and inflammation caused by
depression during the last trimester of pregnancy or postpartum
may contribute to left ventricular heart failure in women with
PPCM or hypertension in women with pre-eclampsia.
The way forward
The aetiology of pregnancy-related cardiovascular complications
in conditions such as pre-eclampsia and PPCM remain unclear.
Depression during pregnancy and the postpartum period is
a common condition. Previous studies have linked perinatal
depression as a risk factor for pre-eclampsia. There is also
evidence in the literature that depression is a risk factor for
and a predictor of poor outcomes in CVD in general. The data
have shown that depression causes an increase in the release
of pro-inflammatory markers such as CRP and IL-6, which
may contribute to the development of CVD, in particular
PPCM. Further studies are required to determine whether
depression in the peripartum period is indeed a risk factor
for cardiovascular complications of pregnancy, for example,
assessing the depression levels in a large group of pregnant
women and then assessing their postnatal outcome.
References
1.
Kamarck W, Stuwart J, Rand K, Muldoon M. A prospective study of
the directionality of the depression inflammation relationship.
Brain
Behav Immunol
2009;
23
(7): 936–944.
2.
Sliwa K, Böhm M. Incidence and prevalence of pregnancy-related heart
Maternal/postpartum depression
Immune response
Cardiovascular
risk
Oxidative stress
Innate
MHC I and II
Inflammatory
cytokines
(IL-6, IL-10
and CRP)
Adaptive
Lipid peroxidation
Pre-eclampsia
Peripartum
cardiomyopathy
Fig. 2.
A hypothetical mechanism by which depression during
pregnancy and postpartum may contribute to the devel-
opment of PPCM and pre-eclampsia.

















