
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
124
AFRICA
using a femoral approach, covering all branches of the arch. The
proximal ends of the stent grafts were positioned in the ascending
aorta above the previously sewn bifurcated graft (in landing zone
0). The distal end of the graft was placed downstream of the
congenital narrowing of the aortic isthmus (Figs 1–3).
Postoperative hospitalisation and rehabilitation proceeded
without complications. A low-dose cardioselective beta-blocker
was used as pharmacotherapy. Thereafter, the patient was under
the care of Heart Surgery Ambulatory.
Despite the above conditions requiring multi-stage treatment,
and the potential complications, the patient consciously decided
to become pregnant and was under the constant supervision
of an experienced cardiologist who specialises in congenital
heart defects in adults. Echocardiography showed normal left
ventricular function (left ventricular ejection fraction
>
50%),
there was no significant gradient of the descending aorta, and
the patient was in NYHA functional class I. The cardioselective
beta-blocker was discontinued. Pregnancy proceeded without
any complications and a decision was made to terminate the
pregnancy at 38 weeks’ duration by caesarean section, after an
interdisciplinary discussion (cardiologist, obstetrician, cardiac
surgeon, neonatologist and patient).
A healthy baby with a birth weight of 2 900 g and 10 points
in the APGAR scale score was transferred to the Department
of Neonatology. The mother spent the first day in the intensive
care unit of Cardiac Surgery. Further hospitalisation proceeded
without any complications and she was discharged home on the
fourth day. Two years after the birth, control vascular imaging
studies confirmed the positive outcome of her previous treatment.
Discussion
Due to different degrees of potential risk for complications
during pregnancy, the European Society of Cardiology (ESC),
in a recent guideline, established a four-scale risk score.
2,3
Our
patient, because of vascular complications, qualified in the third
risk group. A cardiologist, cardiac surgeon and obstetrician
specialising in congenital abnormalities, according to the rules in
force at that time, took care of the gestation.
The decision was made on the date of termination of
pregnancy, taking into account maternal and foetal maturity.
Normally, vaginal delivery has a lower risk of complications and
the use of epidural anaesthesia is the method of choice. This has
been well described in the literature.
4
However in this case, after
interdisciplinary discussion and consultation with the patient,
and based on the 2011 ESC guidelines on the management of
cardiovascular disease during pregnancy,
2
some reports in the
literature,
5,6
and our experience, we decided to terminate the
pregnancy by caesarean section under general anaesthesia.
Conclusion
The most difficult period for cardiac haemodynamics is the
third trimester of pregnancy. Therefore, in the final stage of
pregnancy, patients with a cardiovascular history should be
treated in specialist departments.
References
1. Pu
ś
lecki M, Buczkowski P, Perek B,
et al.
Hybrid procedures for aortic
arch repair.
Kardiochir i Torakochir Pol
2011;
4
: 438–444.
2. Regitz-Zagrosek V, Blomstrom LC, Borghi C,
et al
. ESC guidelines on the
management of cardiovascular diseases during pregnancy: the task force
on the management of cardiovascular diseases during pregnancy of the
European Society of Cardiology (ESC).
Eur Heart J
32
(24): 3147–3197.
3. Trojnarska O, Br
ę
borowicz P, Markwitz W,
et al
. Pregnancy and delivery
in women with congenital heart disease after cardiac surgery.
Arch Med
Sci
2006;
2
: 108–113.
4. Kanakis MA, Mitropoulos FA, Katsetos C, Ntellos C
.
Successful vaginal
delivery in a woman with tetralogy of Fallot and pulmonary atresia after
four cardiac operations.
Hellenic J Cardiol
2012;
53
: 246–248.
5. Balint OH, Siu SC, Mason J,
et al
. Cardiac outcomes after pregnancy in
women with congenital heart disease.
Heart
2010;
96
: 1656–1661.
6. Ross-Hesselink JW, Duvekot JJ, Thorne SA. Pregnancy in high-risk
cardiac conditions.
Heart
2009;
95
: 680–686.
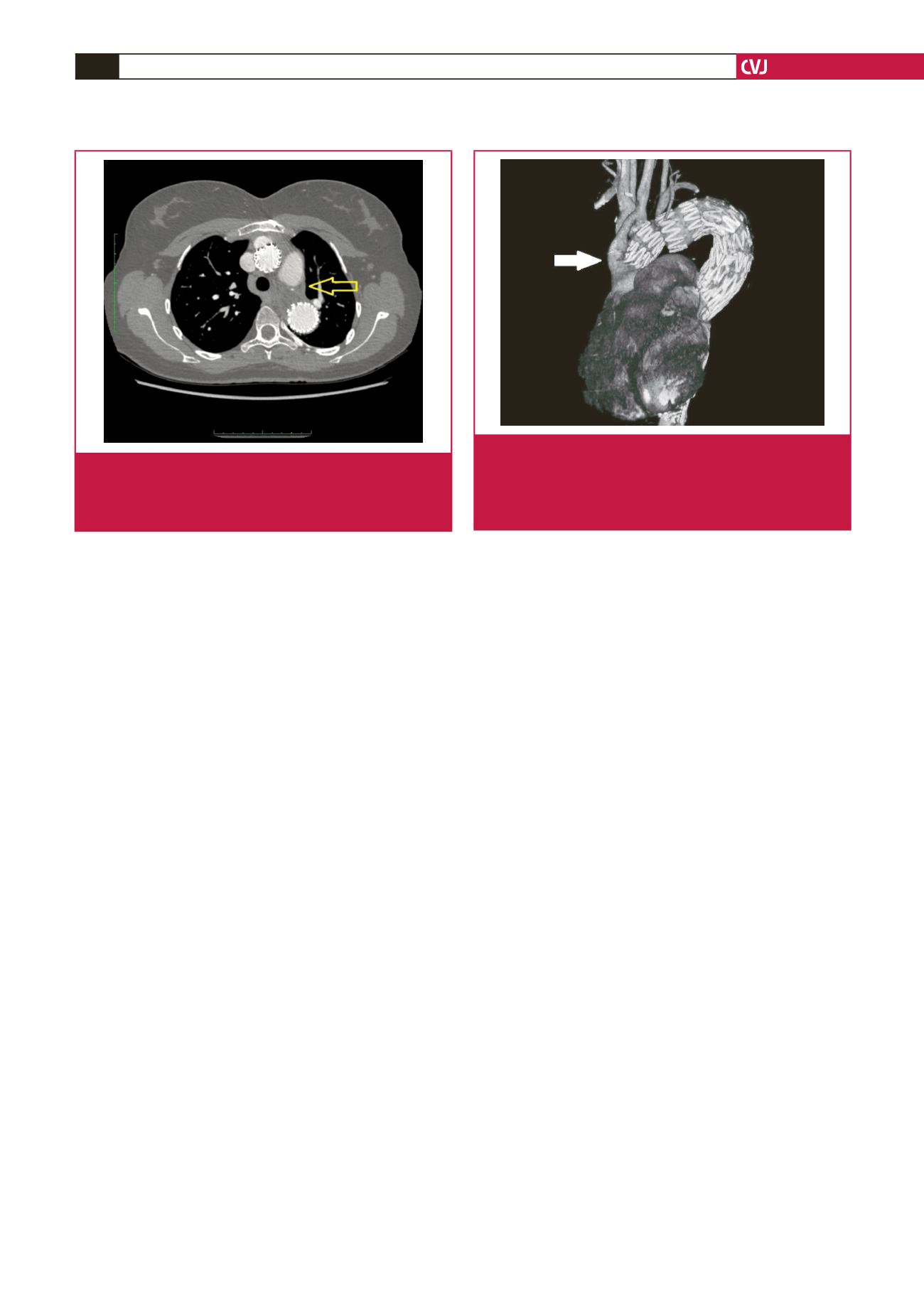
Fig. 3.
Computed tomography angiography, 3D reconstruc-
tion, and current status. This indicates proper function-
ing of the bifurcated graft sewn to the ascending aorta,
proper functioning of the thoracic stent graft, and no
leakage of contrast into the aneurysm sac.
Fig. 2.
Computed tomography angiography two years after
childbirth, four years after the surgery, showing disap-
pearance of the aneurysm sac and correct flow
through the stent graft.

















