
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
62
AFRICA
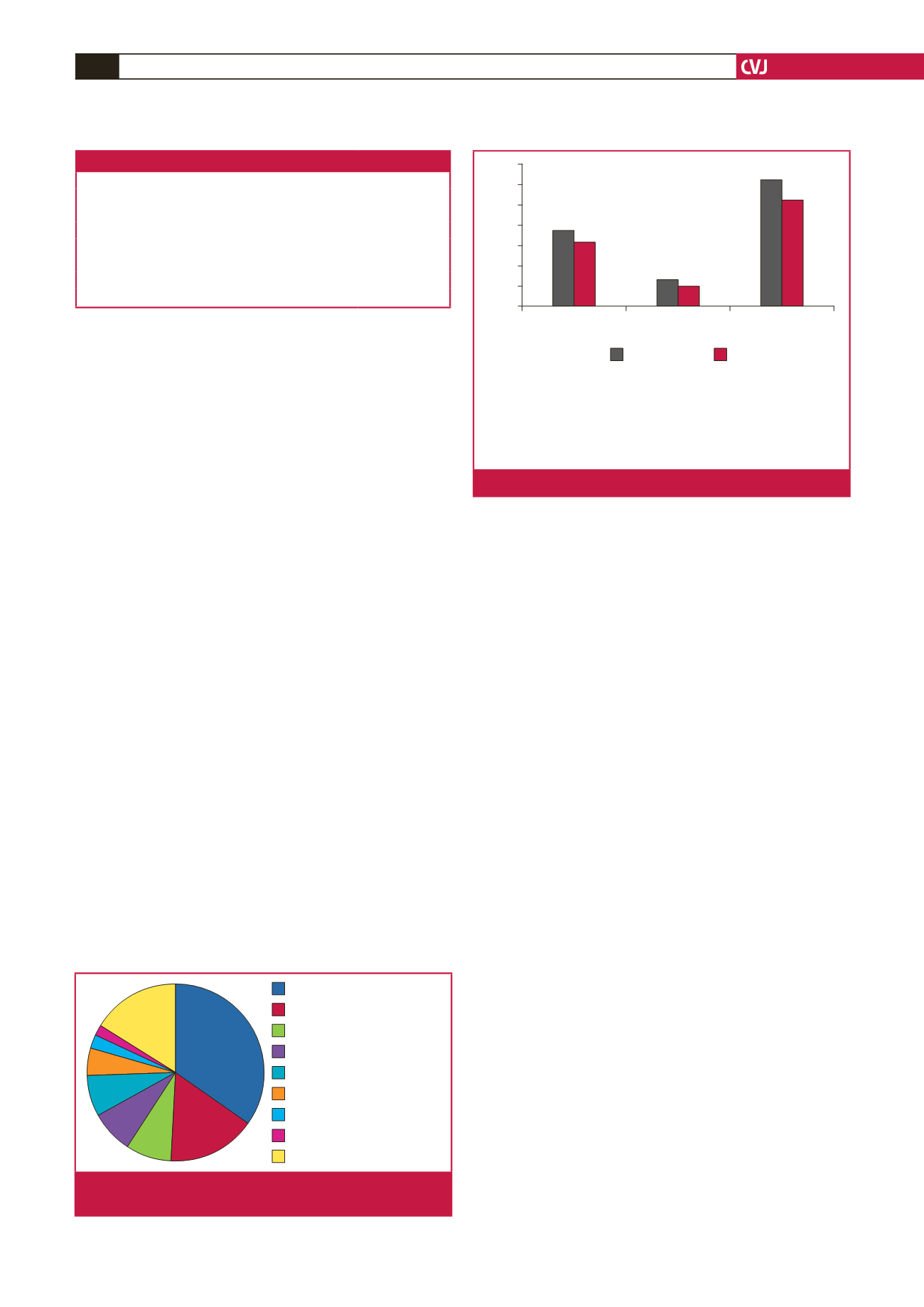
Table 2 summarises the antenatal risk factors (as reported
in the MDNF) as documented at the first antenatal visit of the
pregnant mother. Some patients had more than one risk factor.
Ninety-two (78%) patients attended antenatal clinics, but only
44.3% of patients booked for antenatal care before 20 weeks’
gestation. Fig. 2 describes the level of antenatal care received by
the women who died. Forty (33.7%) mothers delivered vaginally,
31 (26.3%) by Caesarean section, and 47 (39.8%) mothers were
undelivered. The average gestation at delivery was 32 weeks.
Fifty-one (71.8%) babies were born preterm (
<
37 weeks’
gestation). The average birth weight of babies born alive was
2 558 g. Of the babies born alive, 37 (64.5%) were low birth-
weight (
<
2.5 kg) babies.
Cardiovascular conditions and co-morbidities
leading to death
An electrocardiogram and echocardiogram was performed in
only 42.9% (
n
=
50) and 34% (
n
=
40) of patients, respectively.
The mean heart rate of the patients who died was 115 beats per
minute (Table 1); 19 were hypertensive (systolic BP
>
140 mmHg)
and eight were hypotensive (systolic BP
<
100 mmHg).
The majority of women (69%,
n
=
71) died after delivery, while
the remaining 47 (31%) died during the antenatal period. For the
mothers who died in the postpartum period, death occurred
11
±
10.7 days postpartum. Seventy-two per cent of mothers
presented to the health institutions in a critically ill condition,
while 6% of the mothers were dead on arrival. The maternal
deaths occurred at the following health localities: community
health clinics, five patients (4.12%); level one hospital, 25
(21.7%); level two hospitals, 34 (28.9%); level three hospitals, 50
(42.3%) and private hospitals, four (3.1%).
The diagnosis contributing to cardiac death is illustrated in
Fig. 3. PPCM (34%) and complications of RHD, which includes
un-operated cases, as well as cases with prosthetic valve disease
(25.3%), were the most important diagnoses leading to maternal
death.
PPCM and other cardiomyopathy
There were 41 deaths due to PPCM. All cases were newly
diagnosed as none of the maternal records documented a
previous history of cardiomyopathy. Twelve (29.3%) deaths
occurred at level three institutions, 14 (34.2%) at level two
facilities and 15 (36.6%) at level one or community health clinics.
Twenty (48.8%) mothers presented with acute symptoms in the
postpartum period. Death occurred in nine (22.0%) patients who
were undelivered, and 32 (78.1%) were postpartum.
The most important antenatal co-morbidities identified
among the women who died due to a cardiomyopathy were:
hypertension, 22 patients (53.7%), HIV infection, 17 (41.5%)
and anaemia, 15 (36.6%). Twenty (48.8%) mothers however had
a haemoglobin level of
<
10 g/dl when they presented in acute
cardiac failure. In most cases, a clinical diagnosis was made, in
only 12 (30%) cases was an electrocardiogram performed, and
an echocardiogram was done in five (13%) cases to confirm
diagnosis of a cardiomyopathy.
Rheumatic heart disease
There were 35 maternal death files due to complications of RHD
available for assessment. There were 19 cases of valvular heart
disease, four deaths due to complications of prosthetic heart
valves (presumed to be rheumatic in origin in this South African
population), two deaths due to infective endocarditis and five
cases of underlying valvular lesions complicated by pulmonary
hypertension. Mitral stenosis was the most common valvular
lesion contributing to maternal death (
>
50% of cases with
valvular lesions), followed by severe tricuspid incompetence (
n
=
4), mixed mitral valve disease (
n
=
2), aortic stenosis (n
=
2), and
one case of isolated severe mitral regurgitation.
All four patients with mechanical heart valve prostheses
died due to valve thrombosis. Two patients were non-compliant
with anti-coagulant medications. One patient was treated with
Peripartum cardiomyopathy
Prosthetic heart valves
Pulmonary hypertension
Congenital heart disease
Myocardial infarction
Infective endocarditis
Other
Other cardiomyopathies
Rheumatic heart disease
41 (34%)
19 (6.2%)
2 (1.7%)
3 (2.5%)
19 (16%)
10
(8.4%)
9 (7.6%)
9 (7.6%)
6 (5.1%)
Fig. 3.
Cardiovascular conditions contributing to cardiac death
(
n
=
118).
Specialist: a person registered with the Health Professionals Council of
South Africa (HPCSA) in an appropriate speciality.
General practitioner/medical officer: a doctor with a medical degree
registered with the HPCSA.
Professional nurse: a person who is qualified as a midwife.
Advanced midwife: a professional nurse who has completed a further
year of training in midwifery.
Specialist
General practitioner/
medical officer
Advanced midwife/
professional nurse
70
60
50
40
30
20
10
0
%
Number
Fig. 2.
Antenatal care provider.
Table 2. Antenatal risk factors (
n
=
118)
Risk factor
Number (%)
With known heart disease
46 (39.7)
Smoking (past and current)
11 (9.3)
Tuberculosis (past and current)
8 (6.8)
Hypertension
43 (36.4)
Proteinuria in current pregnancy
22 (18.6)
Glycosuria in current pregnancy
12 (10.2)
Anaemia (haemoglobin
<
10 g/l)
30 (26.8)

















