
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 4, July/August 2016
e18
AFRICA
was awake and conscious at about postoperative hour four. A
subsequent neurological examination revealed no pathology and
the patient was extubated.
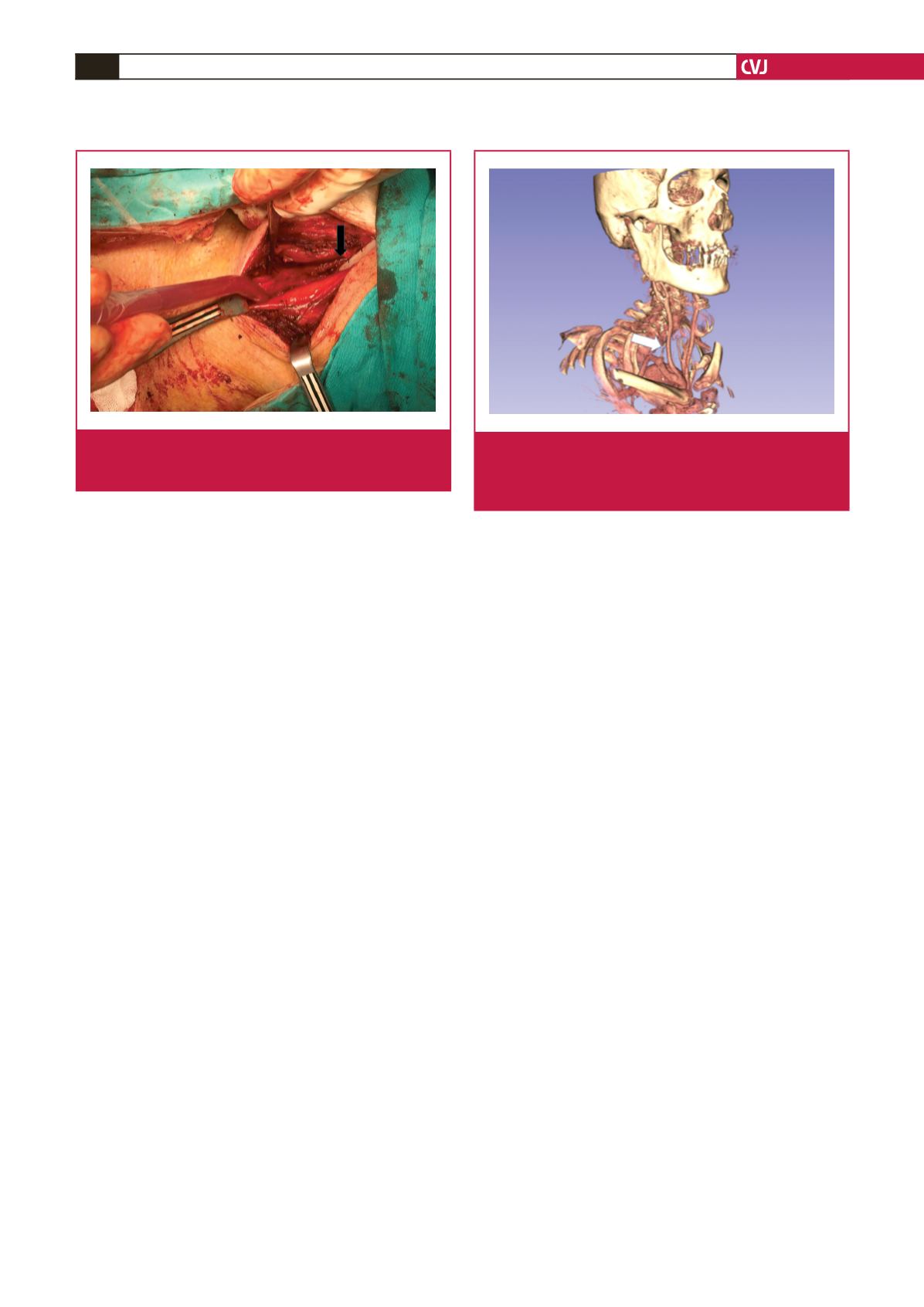
Tomographic angiography performed postoperatively
revealed that the right vertebral artery was present at the outlet
but totally occluded from about 0.5 cm (Fig. 2). The patient
was again examined neurologically but no neurological deficit
was identified. It was therefore recommended that he continue
his treatment of low-molecular-weight heparin. His cardiac
medication and other medical treatment were planned and he
was discharged on condition of follow-up visits.
Discussion
Internal jugular vein catheterisation is preferred in patients
undergoing open-heart surgery, since it is easy to cannulate
and is associated with a reduced risk of complications during
cannulation; it is also distant from the surgical site. The
prevalence of vertebral artery cannulation during internal
jugular vein catheterisation is unknown, probably because there
are fewer cases reported than actually occur. When we reviewed
the literature, it was found to be reported less often than carotid
artery punctures. Carotid artery puncture during internal jugular
vein cannulation has been reported at a rate of 0.5 to 11.4%,
whereas the rate of vertebral artery cannulation was from 0.099
to 0.775%,
2
and fewer than 30 cases were reported on iatrogenic
vertebral artery cannulation.
3
Dissection, thrombosis, formation of arteriovenous fistulae,
and pseudo-aneurysms are complications of vertebral artery
injury during vein cannulation.
3
Diagnosis of pseudo-aneurysm
of the vertebral artery is often delayed because symptoms occur
only late after cannulation.
4
In particular, some patients may
develop fatal vertebrobasilar ischaemia due to vertebral artery
cannulation and associated severe and damaging sequelae, such
as stroke or visual defects, while others may be asymptomatic,
which can be attributed to sufficient extracranial collateral
circulation.
5
The best way to avoid iatrogenic vertebral artery cannulation is
to take the necessary precautions. In other words, the best way to
perform this procedure is under the guidance of ultrasonography,
as recommended in many guidelines. However, this is almost
impossible in emergent cases and when ultrasonography is not
available or is difficult to access. In such cases, intervention may
be performed using anatomical reference points.
The vertebral artery is classically the first branch of the
ipsilateral subclavian artery, and arises from the posterior–
superior part of this artery. The vertebral artery, after separating
from the subclavian artery, generally passes through the
transverse process of the C7 vertebra and superiomedially enters
the transverse foramen of the cervical vertebrae (C6 in 95% of
cases), extending vertically to the level of the C2 vertebra within
the transverse foramen of the vertebrae.
6
The extraforaminal
region is about 4 cm and located deeper and more medially than
the internal jugular vein. It is the region most open to injury, and
in this region it is difficult to stop haemostasis with compression,
7
because the vertebral artery courses in a deep plane.
A safer approach when arterial damage is caused, is with
an immediate surgical or endovascular stent application by
a wide-scale catheter, as stated by Hong-liang
et al
.
8
These
kinds of punctures frequently result from hyperextension of
the neck, accompanied by excessive rotation of the head, or
failure to adjust the direction and depth of the puncture, or
using an excessively long needle to perform the puncture. In
addition, the non-pulsatile flow from the first puncture, due to
the thinner diameter of the vertebral artery, may be misleading.
Both the quantity and colour of the flow are manifested more
clearly when the final tip reaches the subclavian artery following
catheterisation, as in our case.
Conclusion
It should always be considered that during percutaneous
interventions, vertebral artery cannulation may occur, even if
there is only a slight probability. In the event of such a case,
there should be a management plan, previously prepared by the
surgeon and anaesthetists. If endovascular repair is not possible
in vertebral artery catheterisations, or if the artery is completely
Fig. 1.
After foraminectomy the catheter was clearly seen
advancing through the vertebral artery. The black
arrow shows the side of the catheter.
Fig. 2.
Three-dimensional tomographic angiography show-
ing the right vertebral artery was present at the outlet
but totally occluded for about 0.5 cm. The white arrow
shows the right vertebral artery and the occluded part.

















