
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 5, September/October 2016
AFRICA
e1
Case Report
Takotsubo cardiomyopathy post liver transplantation
Ahmed Vachiat, Keir McCutcheon, Adam Mahomed, Gunter Schleicher, Liezl Brand, Jean Botha,
Martin Sussman, Pravin Manga
Abstract
A patient with end-stage liver disease developed stress-
induced Takotsubo cardiomyopathy post liver transplanta-
tion, with haemodynamic instability requiring a left ventricu-
lar assist device. We discuss the diagnosis and management
of this condition.
Keywords:
Takotsubo cardiomyopathy, liver transplantation, left
ventricular assist device
Submitted 25/9/15, accepted 11/3/16
Cardiovasc J Afr
2016;
27
: e1–e3
www.cvja.co.zaDOI: 10.5830/CVJA-2016-032
Case report
A 56-year old male was admitted to hospital for liver
transplantation. He had end-stage liver disease (MELD score
22) due to cirrhosis caused by hepatitis C virus infection and
alcohol abuse. In addition, he had diabetes and was moderately
overweight (body mass index of 32 kg/m
2
). He had no other
risk factors for ischaemic heart disease and had normal renal
function.
Pre-transplant echocardiography revealed a left ventricular
ejection fraction (LVEF) of 75% and moderate pulmonary
hypertension with a systolic pulmonary artery pressure (PAP)
of 41 mmHg. Cardiac catheterisation and coronary angiography
prior to transplantation revealed normal coronary arteries and a
mean PAP of 28 mmHg, falling to 23 mmHg after nitric oxide
inhalation. His pulmonary vascular resistance was found to be
2.05 Wood units.
The patient underwent an orthotopic liver transplantation.
Standard procedure during the transplantation required cross
clamping of the abdominal aorta while the hepatic artery
anastomosis was being performed.
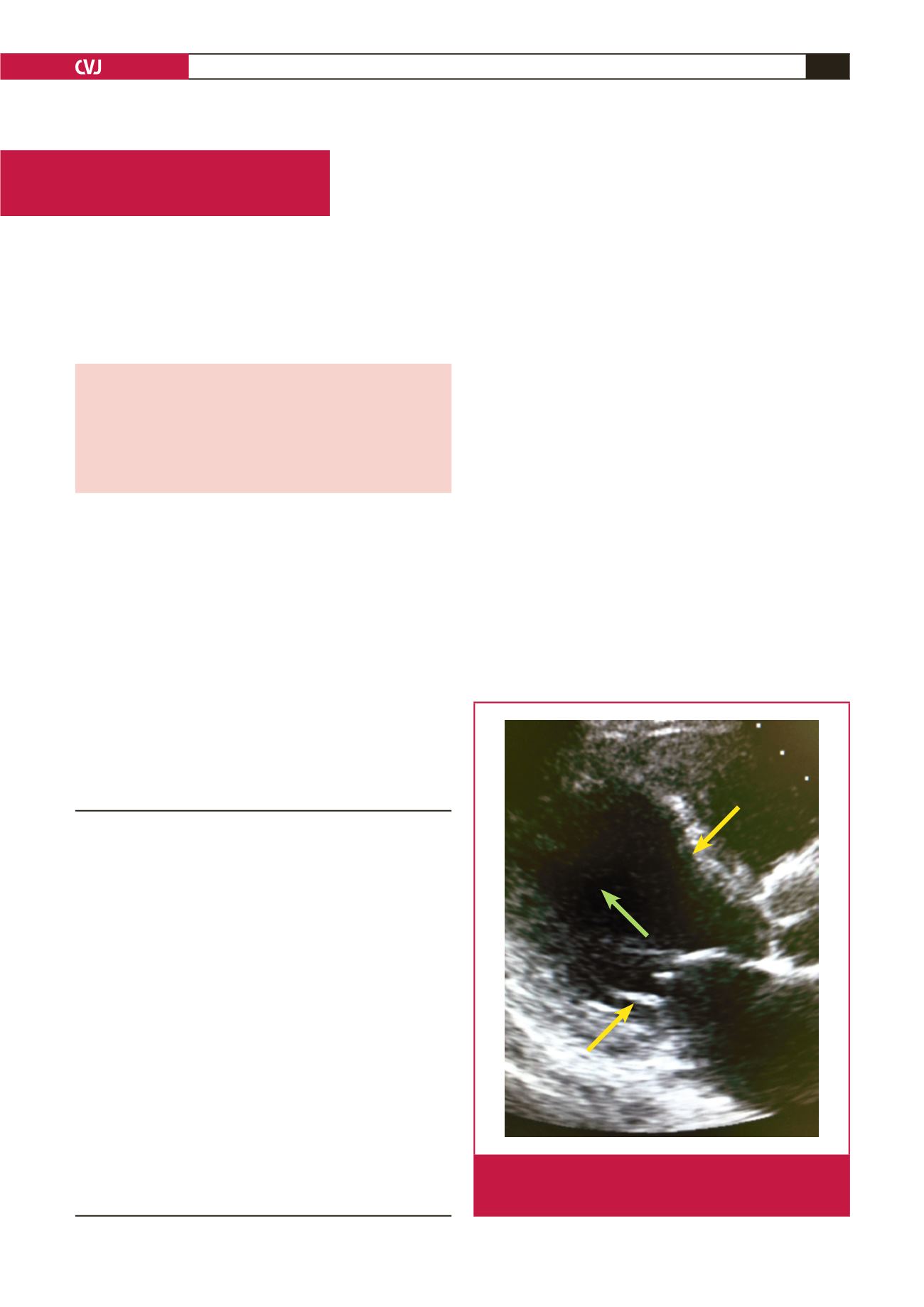
Post transplantation he developed acute left ventricular
dysfunction (LVEF 23%) with apical ballooning and basal hyper-
contractility, which is typical of Takotsubo cardiomyopathy,
requiring inotropic support (Fig. 1). His ECG showed sinus
Division of Cardiology, Department of Internal Medicine,
University of Witwatersrand and Charlotte Maxeke
Johannesburg Academic Hospital, Johannesburg, South
Africa
Ahmed Vachiat, MB BCh (Wits), FCP (SA), MMed, Cert Cardiology
(SA),
Ahmed.Vachiat@wits.ac.zaPravin Manga, MB BCh (Wits), FCP (SA), PhD
Keir McCutcheon, BSc (Hons), MSc, MB BCh (Wits), FCP (SA),
Cert Cardiology (SA)
Adam Mahomed,MB BCh (Wits), FCP (SA), Cert Gastroenterol (SA)
Wits Donald Gordon Medical Centre, University of
Witwatersrand, Parktown, Johannesburg, South Africa
Ahmed Vachiat, MB BCh (Wits), FCP (SA), MMed, Cert Cardiology
(SA),
Ahmed.Vachiat@wits.ac.zaPravin Manga, MB BCh (Wits), FCP (SA), PhD
Keir McCutcheon, BSc (Hons), MSc, MB BCh (Wits), FCP (SA),
Cert Cardiology (SA)
Adam Mahomed,MB BCh (Wits), FCP (SA), Cert Gastroenterol (SA)
Gunter Schleicher,MB BCh (Wits), DTM&H, MMed, FCP (SA), Cert
Pulmonology (SA)
Liezl Brand, MB ChB (Stell), FCP(SA), Cert Pulmonology (SA)
Jean Botha, MB BCh (Wits), FCS (SA)
Milpark Hospital, Parktown, Johannesburg, South Africa
Martin Sussman, MB BCh (Wits), FCS (Cardiothoracic Surgery)
Fig. 1.
Parasternal long-axis view showing apical and mid-
cavity ballooning (green arrow) and basal hyper-
contractility (yellow arrows).

















