
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 5, September/October 2016
AFRICA
e5
mg, spironolactone 25 mg, warfarin 1.25 mg, and a single dose
of 400 mg albendazole. Despite improvement with resolution
of dyspnoea and chest pain after 24 hours, the patient died
unexpectedly on day 6 while sleeping.
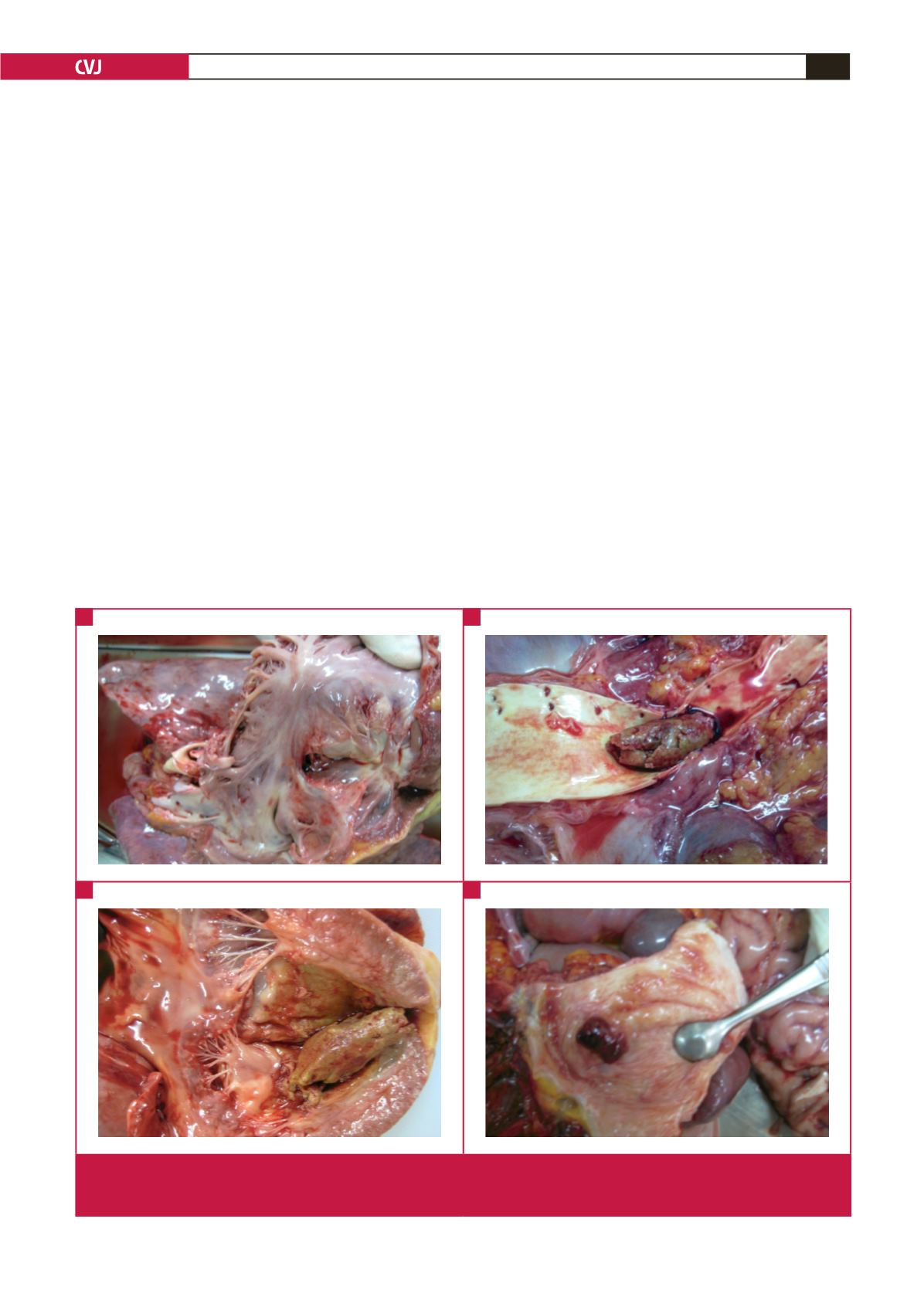
Autopsy confirmed right ventricular diffuse endocardial
fibrous thickening with amputation of the apex (Fig. 1A),
aneurysmal dilatation of the right atrium, and extensive
endocardial fibrosis of the left ventricle. The bifurcation of the
aorta was filled with a large embolus (Fig 1B) that could have
been seated at the left ventricular apex (Fig 1C). The bladder
revealed active polypoid bilharzial cystitis (Fig 1D).
On microscopy, typical endocardial fibrous thickening (Fig.
2A) and eosinophilic granulomas centred by viable
Schistossoma
eggs were found (Fig 2B). Additional features were chronic
passive congestion of the liver, spleen and lung, as well as hepatic
periportal fibrosis with the presence of eosinophilic granulomas.
Discussion
This patient, coming originally from a known endemic region
for EMF, had bilateral disease. He had concurrent signs of
severe endocardial fibrosis, marked tissue hyper-eosinophilia and
active
Schistosoma haematobium
granuloma in the bladder. He
therefore presented with signs of both chronic EMF and active
schistosomal infestation, as defined by the presence of viable
eggs and active granuloma.
The patient had been relatively asymptomatic until three
months prior to admission, in marked contrast with the severity
of the echocardiographic and pathological features. Discrepancy
between echocardiographic and clinical findings is not
uncommon,
2
and recent schistosomiasis may have contributed to
aggravation of a stable chronic EMF.
Although emergency surgery had been considered when the
child was admitted, it was not performed due to the presence
of extensive endocardial fibrosis with severe ventricular cavity
amputation, pulmonary hypertension and electrocardiographic
signs of myocardial ischaemia, all predictors of a bad prognosis.
Since antithrombotic therapy was unavailable, the child was
treated with warfarin only. Sudden death occurred probably due
to ventricular arrhythmia that may have been determined by
dislodgment of the large apical left ventricular thrombus and
embolisation to the aortic bifurcation.
Loffler’s syndrome is used as a model to explain some clinical–
pathological features of EMF,
3
but eosinophilic myocarditis
is rarely proven in these patients. Endomyocardial biopsy is
rarely performed due to lack of expertise and non-existence of
adequate facilities for catheterisation in endemic areas, as well as
the presence of advanced disease and intracavitary thrombi, as
Fig. 1.
Typical features of right ventricular EMF include fibrosis and retraction (A). A large embolus that could have been seated at
the left ventricular apex (B) is seen at the bifurcation of the abdominal aorta. Macroscopic evaluation also revealed extensive
left ventricular endocardial fibrosis (C) and bilharzia polypoid cystitis (D).
C
A
D
B

















