
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 6, November/December 2016
AFRICA
351
recognised as an acceptable standard of therapy, and the choice
of adjuvant treatment varies significantly among experts in the
field.
Colchicine is an inhibitor of microtubule polymerisation. It
acts by binding to tubulin and is registered for the acute treatment
of gout crystal arthropathies. The plant source of colchicine,
the autumn crocus (
Colchicum autumnale
),
was described as
treatment for arthritis in the
Ebers Papyrus
in 1500 BC.
12
In
modern medicine, colchicine has however played a wider role in
the treatment of pericarditis of various aetiologies, both acute and
chronic. This has been investigated in a prospective, randomised
trial named COPE (Colchicine for Acute Pericarditis),
13
and the
major findings concluded that colchicine significantly reduced
the recurrence rates and symptom persistence due to pericarditis.
To date however, the use of colchicine has, to the best of our
knowledge, never been systematically assessed in the context of
pericardial TB. The purpose of this research was to assess the
merit for the use of colchicine in the context of TB pericarditis.
Methods
This research was conducted in the Northern Cape province of
South Africa at a secondary-level hospital in Kimberley between
August 2013 and April 2015. The research was approved by
the ethics committee of the University of the Free State and
the study was registered with the National Health Research
Committee. The research was conducted in accordance with the
Declaration of Helsinki.
This pilot study was designed as a prospective, double-
blind, randomised, control cohort. All patients presenting
to the Kimberley Hospital complex (KHC) with pericardial
effusions were assessed for inclusion and exclusion criteria.
In the absence of contra-indications, patients underwent
therapeutic pericardiocentesis if the procedure was deemed
safe and possible. Standard therapy was initiated in accordance
with the South African National Tuberculosis Management
Guidelines:
14
weight-adjusted anti-TB drugs (Rifafour
®
) and
oral corticosteroids. (prednisone: 1.5 mg/kg per day for four
weeks; 1.0 mg/kg per day for two weeks; 0.5 mg/kg per day for
one week; 0.25 mg/kg per day for one week). HIV co-infected
patients not previously on treatment were initiated on fixed-
dose combination (FDC) antiretroviral treatment six weeks
after initiation of TB treatment (FDC: Tenofovir Disoproxil
Fumarate 300 mg, Emtricitabine 200 mg and Efavirenz 600 mg).
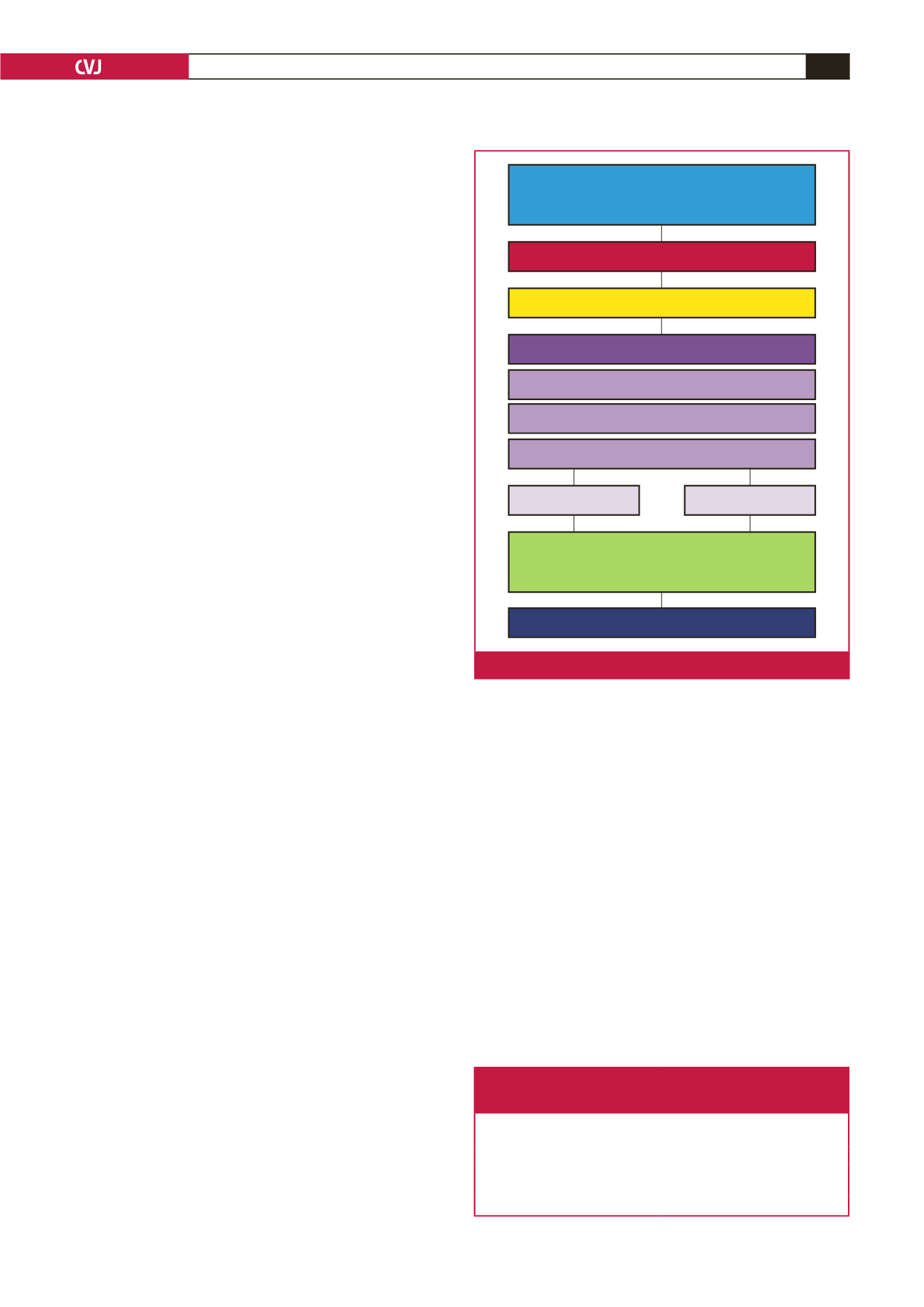
Patients were randomly assigned to the intervention group
with the use of a web-based randomisation system that ensured
assignment concealment. The intervention group received
colchicine (dose 1.0 mg per day) for a total of six weeks, whereas
the control group received a placebo for the same period (Fig. 1).
Patients subsequently underwent serial echocardiographic
examinations on an out-patient basis and adherence checks,
including pill counts, were done at follow-up visits. The
primary outcome assessed was the development of pericardial
constriction and this diagnosis was made echocardiographically
at four months post initial presentation. Upon completion of the
follow-up period of all patients, the blinding was unveiled and
data were presented for statistical analysis.
Two groups of patients were included: (1) definite TB
pericarditis: the presence of TB bacilli was observed on
microscopic examination of pericardial fluid; cultures of
pericardial fluid were positive for Rifampicin-sensitive
Mycobacterium tuberculosis
(MTB); pericardial fluid was positive
for MTB on direct polymerase chain reaction (PCR) (Gene
Xpert); and (2) probable TB pericarditis: proof of TB was found
elsewhere (positive cultures for MTB on sputum or cerebrospinal
fluid); pericardial fluid with adenine deaminase (ADA) level >
40 U/l; a total diagnostic index score > 6 on using the Tygerberg
clinical prediction score (Table 1).
15
The exclusion criteria were: patients with renal or hepatic
impairment (creatinine clearance rate < 85 ml/min or
transaminases > 1.5 upper limit of normal); and pregnant
patients or patients intending to become pregnant within four
months.
The gold-standard diagnostic test for the diagnosis of CP is
the demonstration of increased interventricular interdependence
during cardiac catheterisation. Doppler echocardiography and
other novel echocardiographic techniques have provided us
with reliable non-invasive alternatives to the diagnosis of CP.
Table 1.The Tygerberg clinical prediction score for the diagnosis of TB
pericarditis. A total diagnostic score > 6 yields a sensitivity of 82%
and a specificity of 76% for the diagnosis of TB pericarditis
Admission variable
Diagnostic index
Weight loss
1
Night sweats
1
Fever
2
Serum globulin
>
40 g/l
3
Leukocyte count
<
10
×
10
9
3
Patients presenting to Kimberley Hospital with
pericardial effusion (Aug 2013–Dec 2014)
(
n
=
72)
Assessment for inclusion and exclusion criteria
Study participants (
n
=
33)
Baseline Investigation
Pericardiocentesis if deemed safe
Standard therapy
Double-blinded randomisation
Statistical analysis
Follow-up echocardiography.
Primary outcome: pericardial constriction.
Colchicine (
n
=
19)
Placebo (
n
=
14)
Fig. 1.
Flow diagram illustrating study methodology.

















