
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 6, November/December 2016
AFRICA
353
The study population had a female preponderance (66%
females) and the mean age of the studied patients was 31 years.
Disseminated pericardial tuberculosis was found to be a disease
exclusive to the immune-compromised in this cohort; all 21
patients were HIV positive. The median CD4
+
count was 162 and
346 cells/mm
3
in the colchicine and placebo groups, respectively.
Of the 21 eligible participants, 12 had been assigned to the
treatment group and the remaining nine were in the placebo
group. The diagnosis of definite
pericardial tuberculosis was
made in 23.8% of the patients, while the remaining 76.2% were
diagnosed on the basis of suggestive clinical and biochemical
features (see inclusion criteria). Of the studied patients, 47.6%
underwent pericardiocentesis, whereas the remaining 52.4%
could not undergo safe pericardiocentesis.
The average volume of fluid drained via single pericardial
aspiration was 622 ml. The macroscopic appearance of the fluid
varied from serosanguineous to haemorrhagic, reflecting the
different pathological stages of development.
Mycobacterium
tuberculosis
was proven on pericardial aspirates in 50% of cases,
either by positive culture (30%) or by direct PCR technique
(Gene Xpert) (20%) (Table 2).
Pericardial constriction is the natural sequela of
approximately 17 to 40% of TB pericardial infections.
3
In our
cohort, the incidence of pericardial constriction (demonstrated
by echocardiography) four months after the initial diagnosis
was 23.8%. Of the five patients who developed pericardial
constriction, two were in the control group and the remaining
three were in the group treated with colchicine. Of those who did
not develop pericardial constriction, nine were in the colchicine
group and seven were in the placebo group.
The data from Table 3 yields a
p
-value of 0.88. The relative risk
for developing constriction in the colchicine group compared to
the intervention group was 1.07 (95% CI: 0.46–2.46). There was
therefore no statistically demonstrable correlation between the
use of colchicine and pericardial constriction in this study cohort.
The side effects among the patients using colchicine were
usually minor; 56% of the initial 19 patients who were in the
colchicine group reported self-limiting diarrhoea during their
hospital stay. Serious side effects were observed in one patient
who developed hepatitis during his course of treatment. The
patient was removed from the study and daily liver function
testing showed a rapid recovery.
Although the study was neither empowered nor designed
to evaluate the effect of pericardiocentesis on the subsequent
development of pericardial constriction, a very apparent and
interesting finding was observed. We found that, with the
exception of one patient, all those who developed pericardial
constriction were in the group that did not undergo
pericardiocentesis. Conversely, in the group that underwent
pericardiocentesis, only one participant developed pericardial
constriction. Pericardiocentesis therefore seemed to be very
effective in the prevention of pericardial constriction and in this
cohort only one patient (10%) who underwent pericardiocentesis
developed constriction. These findings are observational and
disregard the initial group allocations.
Discussion
The proverbial ‘eureka moment’ in the management of TB
pericarditis seems to be elusive. Numerous interventions have
been postulated and investigated in an attempt to prevent
the devastating post-inflammatory changes in the pericardium
following TB pericarditis. In this pilot study, the merit of adding
colchicine to the current management guidelines was investigated
in a systematic manner. As all the participants of this study were
HIV positive, the findings can only be applied to this subgroup
of patients with TB pericarditis.
There was a notable difference in the median CD4
+
lymphocyte count between the treatment and placebo groups,
but when assessed as an independent variable, no correlation
could be demonstrated between degree of immunocompetency,
as measured by CD4
+
count, and the risk for development of
constriction.
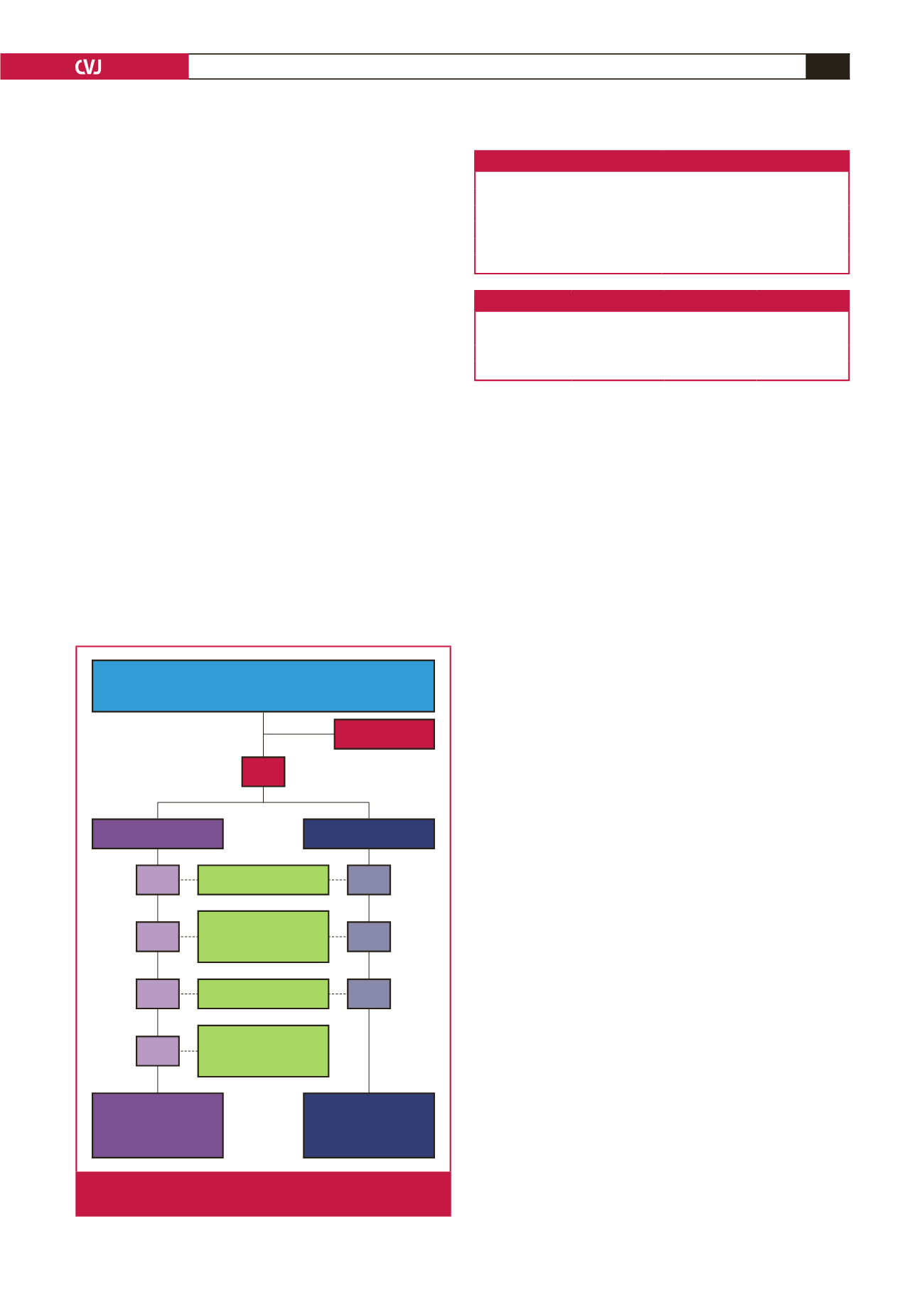
72 patients screened
August 2013 – April 2015
In-patient deaths
Lost to follow-up
Deaths during
follow-up period
1 drug induced
liver injury
39 not eligible
33
19 colchicine group
Total: 12 patients
completing follow
up (colchicine)
14 placebo group
Total: 9 patients
completing follow
up (placebo)
2
1
1
2
1
3
2
Fig. 5.
Screening, randomisation, follow up and analysis of
the study patients.
Table 2. Pericardial fluid biochemistry
Biochemical parameter
Average
Protein (g/l)
62.7
ADA (U/l)
96.6
LDH (U/l)
4494
pH
7.3
Glucose (mmol/l)
2.8
Table 3.Two-by-two table demonstrating the primary study outcome
Colchicine
Placebo
Total
Constriction
3
2
5
No constriction
9
7
16
Total
12
9
21

















