
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 6, November/December 2016
352
AFRICA
In this study, the diagnosis of CP was made by means of
echocardiography by adhering to the principles in the article by
Dal-Bianco
et al
. on the echocardiographic diagnosis of CP.
16
Initial echocardiographic assessment ensured that no features
of constriction were present at the time of enrolment in the
study. Follow-up echocardiograms were performed four months
after the initiation of therapy.
The echocardiograms were performed and co-reviewed by
two experienced echocardiographers (who had both attended
a dedicated workshop at a tertiary-level academic hospital
aimed at the echocardiographic diagnosis of CP). A GE Vivid
E6
®
ultrasound machine was used to perform a systematic
examination according to the basic minimum standards
as stipulated by the British Society of Echocardiography.
17
Numerous other echocardiographic parameters were assessed,
including the presence of a septal shudder, respiratophasic septal
shift, left atrial enlargement and echocardiographic features of
pericardial thickening (Figs 2–4).
Statistical analysis
Statistical analysis was performed by the Department of
Biostatistics of the University of the Free State, Bloemfontein,
South Africa. The SAS Version 8.3 was used. Groups were
compared regarding outcomes using frequency tables with
appropriate hypothesis testing (chi-squared of Fisher’s exact test)
and 95% confidence intervals for differences in percentages. The
standard deviation value
p
< 0.05 was considered significant.
Results
Thirty-three patients met the initial inclusion criteria. Three
patients passed away while in hospital and an additional three
passed away during the follow-up period. In-patient deaths
were due to neutropenic sepsis, cerebrovascular incident and
nosocomial pneumonia, respectively. In all out-patient deaths,
the cause was undetermined. Five patients were lost to follow up
and one patient was removed from the study due to presumed
drug side effects. A total of 21 patients completed the follow-up
period (Fig. 5).
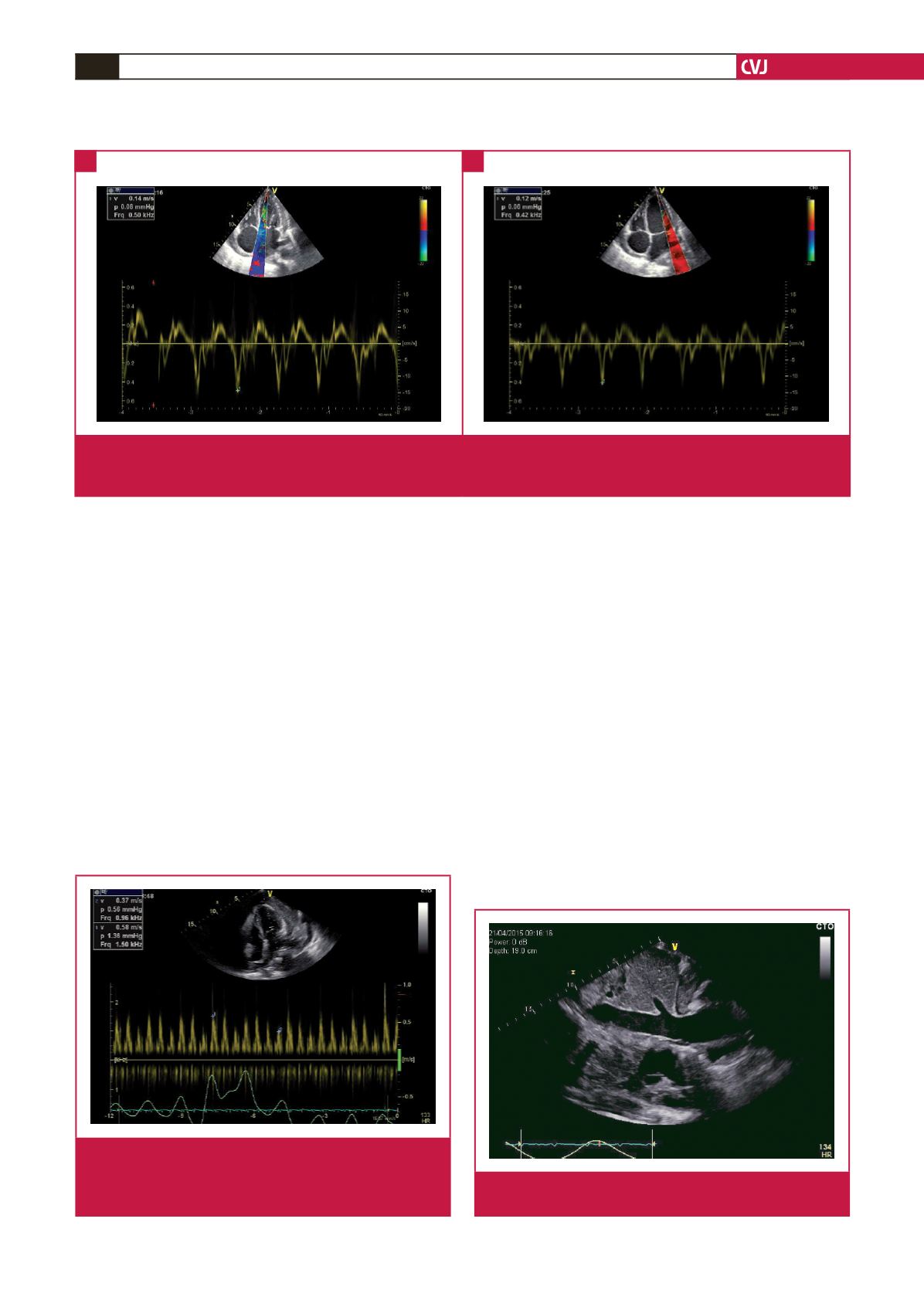
Fig. 2.
A. Tissue Doppler of the medial aspect of the mitral valve annulus demonstrating early diastolic tissue velocity of 0.14 m/s. B.
Tissue Doppler of the lateral aspect of the mitral valve annulus showing early diastolic tissue velocity of 0.12 m/s. The lower
tissue velocity on the lateral aspect is the opposite of the normal phenomenon (annulus reversus).
A
B
Fig. 3.
Pulse-wave Doppler at the level of the mitral valve
leaflet tips demonstrating a respiratophasic variation
in the early diastolic transmitral inflow velocities in
excess of 25%.
Fig. 4.
Dilated and distended inferior vena cava. No respira-
tory variation was observed.

















