
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 6, November/December 2016
390
AFRICA
specifically HbA
1c
level, ambulatory BP and silent ischaemia in a
bi-ethnic gender cohort. Overall, African men showed a poorer
cardiometabolic profile accompanied by lower cortisol levels
when compared to their Caucasian counterparts. Attenuated
cortisol levels therefore seem to act as the driving force in the
cortisol:BDNF ratio and may ultimately down-regulate BDNF.
The novel ratio of cortisol:BDNFmay sustain cardiometabolic
risk and induce neurodegeneration. Cardiometabolic morbidity
further increased in the African men as their reduced coronary
perfusion, as evidenced in the number of 24-hour silent ischaemic
events, would increase BP as a compensatory mechanism to
maintain homeostasis.
Despite the fact that a pre-diabetic state was demonstrated
in the African gender cohort, it was not directly associated with
cortisol:BDNF ratio. In another SABPA sub-study, chronic
hyperglycaemia was shown to facilitate endothelial dysfunction
and susceptibility to stroke risk in the African male cohort.
17
Indeed, Hamer
et al
.
18
also demonstrated associations between
glucose homeostasis as assessed by HbA
1c
concentration and
coronary artery calcification. A hyperglycaemic state therefore
predisposes to cardiometabolic morbidity in the presence of
emotional distress markers such as cortisol:BDNF.
A profile of blunted cortisol and norepinephrine metabolite
responses were associated with structural wall remodelling in a
depressed SABPA African male cohort.
12
The attenuated cortisol
levels of the current African sub-group may therefore support
the notion of increased chronic distress.
19,20
Attenuated BDNF levels in Africans might also induce
decreased neuroplasticity, vulnerability to depression and
cardiovascular risk.
6
In this study, cortisol:BDNF ratio was
associated with silent ischaemia, suggesting possible down-
regulation of BDNF, and implicating a central neural regulatory
role.
10
In animal studies, high concentrations of BDNF in
hypothalamic nuclei and neurons secreting CRF support the
role of BDNF in the stress response.
6
During chronic stress,
a maladaptive cortisol response is elicited due to structural
changes in the HPA axis.
21-23
A state of psychological distress in
Africans may therefore be present.
12,19,20
Indeed, we have confirmed that chronic depression in
the SABPA African teachers’ cohort was associated with
microvascular dysregulation and perfusion deficits.
21
If this
state is further supported by high levels of alcohol abuse,
the central depressant effect of alcohol may disturb central
cardiometabolic homeostasis.
21
Chronic psychological stress
induces sympathetic hyperactivity,
17
higher circulating levels of
catecholamine and cortisol, and ultimately down-regulation
will occur.
12,22-24
Therefore, the lower cortisol level may act as the
driving force behind a possible down-regulated BDNF.
The cortisol:BDNF ratio in African men suggests a
susceptibility to increased cardiometabolic risk. Indeed,
cortisol:BDNF is associated with silent ischaemia in African men
and impairs central autoregulation, explaining the compensatory
increases in blood pressure to maintain homeostasis.
3,14,19
During chronic stress, sympathetic hyperactivity and increased
norepinephrine and cortisol levels will elicit vasoconstrictive
responses and reduce perfusion in the coronary circulation.
12,23
Furthermore, susceptibility to emotional distress as well
as HPA-axis disturbance is enhanced when using defensive
coping mechanisms.
14
Defensive coping facilitated autonomic
dysfunction or sympathetic hyperactivity in the current African
male cohort.
14
This underpins the importance of a central
regulatory control system where higher emotional demands
impact on cardiometabolic health.
Cortisol can further induce or exacerbate down-regulation
of BDNF during chronic stress conditions.
6,10
Lower levels of
BDNF have been associated with depression,
6
and recently
cardiometabolic risk.
10
Down-regulation and the aftermath of
low BDNF levels impair neuroplasticity and homeostasis.
11,13,23,24
With BDNF down-regulation, dysregulation of the HPA axis
may also occur, as both BDNF and cortisol critically impact
on the stress response.
24
This suggests that central neural
control dysregulation enforces a disturbed cortisol:BDNF ratio,
augmenting silent ischaemia and overburdening the heart. This
is the first time this ratio has been reported, and further research
is needed to support the findings and significance.
Susceptibility to emotional distress may be an underlying
factor in the observed differences in the bi-ethnic gender cohort.
We suggest that attenuated cortisol levels may act as the driving
force to downregulate BDNF, increasing cardiometabolic risk
and reducing coronary perfusion during psychological distress.
One limitation of the study is that a very specific population
was studied and results may vary across populations, depending
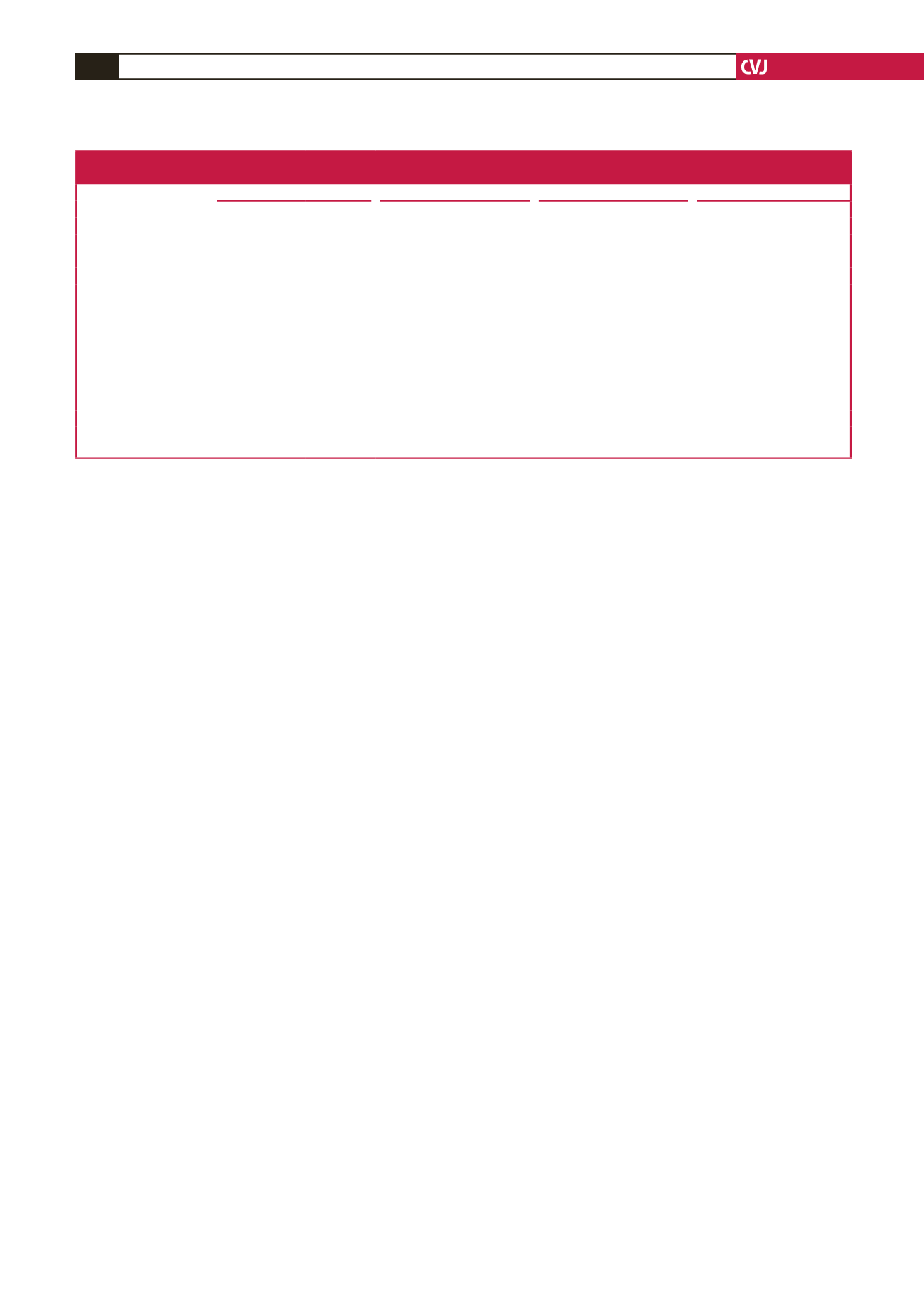
Table 4. Independent associations between cardiometabolic risk markers,
cortisol as well as cortisol:brain derived neurotrophic factor (BDNF) in an African male cohort
HbA
1c
24-h SBP
24-h DBP
Silent ischaemia
β
(95% CI)
p-
value
β
(95% CI)
p-
value
β
(95% CI)
p-
value
β
(95% CI)
p-
value
Adjusted
R
2
0.16
0.29
0.21
0.12
Cortisol
0.21 (0.0–0.4)
0.04
0.23 (0.1–0.4)
0.01
0.23 (0.1–0.4)
0.01
0.18 (0.0–0.4)
0.07
GGT
–
0.14 (0.0–0.3)
0.10
0.22 (0.0–0.4)
0.02
–
Age
–
0.30 (0.1–0.5)
<
0.01
0.20 (0.0–0.4)
0.04
0.33 (0.1–0.5)
<
0.01
Log physical activity
–
0.30 (0.1–0.5)
0.02
0.28 (0.0–0.5)
0.08
–
Body surface area
–
0.18 (–0.1–0.4)
0.14
0.15 (–0.1–0.4)
0.26
–
Adjusted
R
2
<
0.10
0.26
0.15
0.22
Cortisol:BDNF
0.20 (0.0–0.4)
0.03
–
–
0.40 (0.2–0.6)
<
0.01
Log cGGT
–
–
–
–
Age
0.32 (0.1–0.5)
<
0.01
–
–
0.36 (0.2–0.5)
<
0.01
Log physical activity
0.29 (0.0–0.5)
0.02
–
–
0.16 (0.0–0.4)
0.09
Body surface area
0.21 (0.0–0.5)
0.09
–
–
–
HbA
1c,
glycated haemoglobin; SBP, systolic blood pressure; DBP, diastolic blood pressure; log cGGT, log gamma-glutamyl transferase.
Additional covariates included log cotinine levels.

















