
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 6, November/December 2016
396
AFRICA
CAD or at high risk thereof, smoking cessation, avoidance of
excess alcohol intake, an ACE-I for patients with asymptomatic
LVSD, and beta-blockade for those with LVSD after MI.
Heart failure is defined as appropriate symptoms, possibly
accompanied by physical signs of congestion, with evidence
of structural heart disease on echocardiography. The guideline
includes a new category of heart failure with mid-range ejection
fraction (HFmrEF) of 40–49% in the range between heart failure
with reduced ejection fraction (HFrEF) and heart failure with
preserved ejection fraction (HFpEF). Treatment of HFmrEF is
yet to be clearly defined.
ProBNP is more important in ruling out heart failure than in
proving the diagnosis. Novel additions to the guidelines are the
use in appropriately selected patients of an angiotensin receptor
neprilysin inhibitor (ARNI) (sacubitril-valsartan) to replace
ACE-I, cardiac resynchronisation therapy (CRT), and ivabradine
should they remain symptomatic on ACE-I/ARB, beta-blockade
and MRA treatment. HFpEF and HFmrEF should be treated
symptomatically, using diuretics to relieve congestive symptoms.
The guideline discusses at length various co-morbidities and
their management in the setting of heart failure.
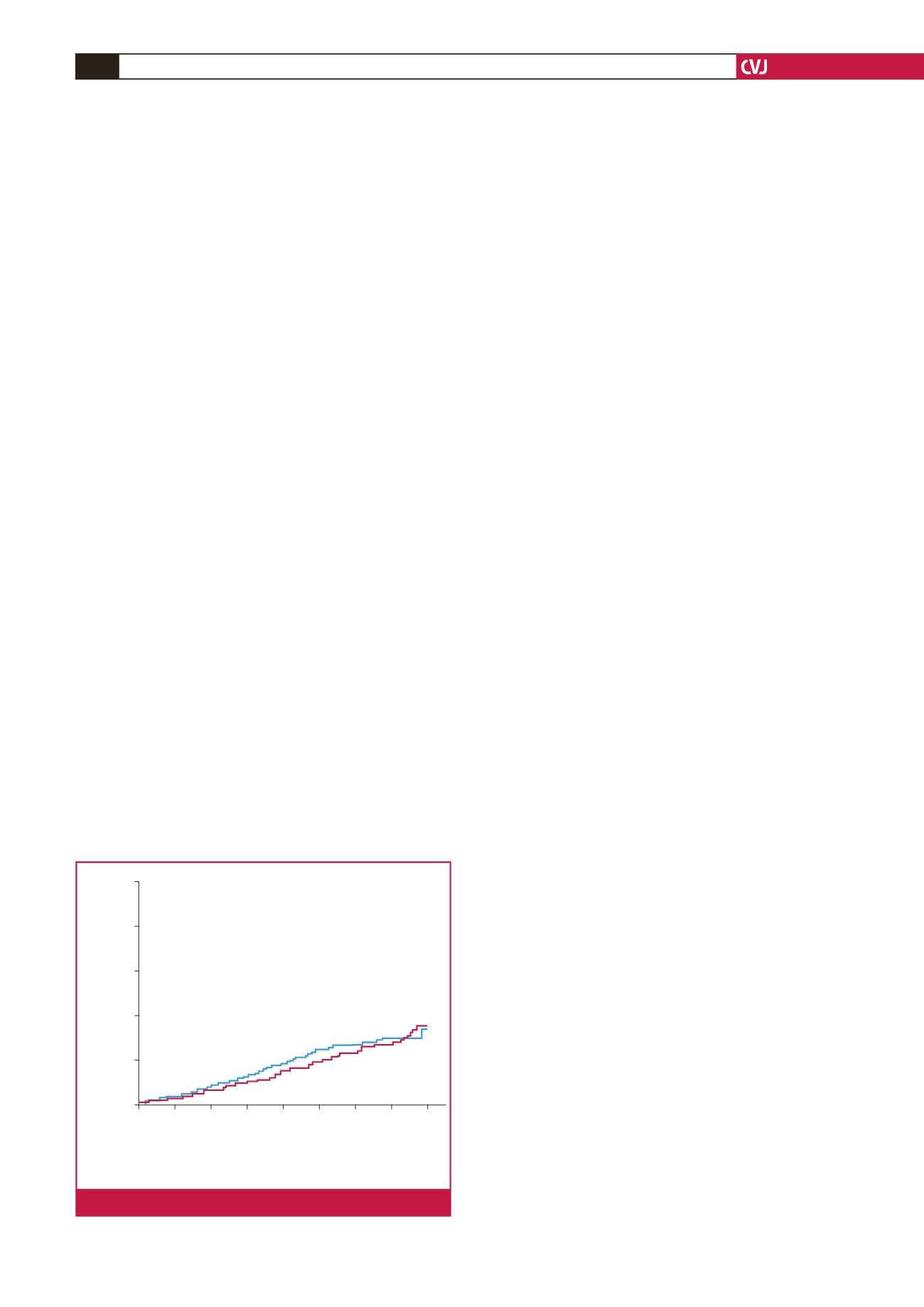
A ‘hotline’ session was devoted to device interventions
in heart failure. The DANISH study evaluated the use of
implantable cardioverter defibrillators (ICDs) in non-ischaemic
heart failure in patients with NYHA class II to III symptoms
and an ejection fraction
<
35% (Fig. 2).
21
The study did not
achieve its primary endpoint of reducing mortality rates. There
was a reduction in incidence of sudden death and a reduction in
total mortality rate in the subgroup under 60 years of age. Two
other studies, REM-HF and MORE-CARE, reported on remote
monitoring for worsening heart failure. Both failed to show any
improvement in outcome.
Another two studies on cell therapy in heart failure could not
demonstrate any benefit.
Cardio-oncology
This is an emerging area of concern for cardiologists and
oncologists alike, given the increasing numbers of patients who
may now survive for years after cancer treatment. The heart
and blood vessels may be affected in a variety of ways by either
chemotherapy or radiation. Myocardial dysfunction and heart
failure, CAD, valvular heart disease, pericardial involvement,
arrhythmias, hypertension, pulmonary thromboembolism, stroke,
peripheral vascular disease or pulmonary hypertension may
occur, not only acutely but also after a delay of months or years.
The patient’s presentation is influenced by the agent used,
the dose and duration of treatment, age, kidney function and
pre-existing CV disease. Myocardial toxicity is of particular
concern and its early detection, as evidenced by deteriorating
LVSD on echocardiography in comparison to baseline values
and/or by elevation in hs-troponin T, is important. Baseline
echocardiography with follow up at the completion of treatment
and then at three and six months is recommended. ACE-I or
ARB, beta-blocker and MRA therapies are cardioprotective as
well as effective in managing overt heart failure. Not all patients
recover normal left ventricular function after the cessation of
treatment. In those who do, it may be possible to discontinue the
cardioprotective treatment.
22
Atrial fibrillation
Apart from death and stroke, the ESC 2016 guideline includes
recognition of hospitalisations, left ventricular dysfunction
and heart failure, cognitive decline and vascular dementia, and
impaired quality of life as consequences of AF. An algorithm is
provided for the detection of AF in patients with an implanted
device presenting after detection of a high atrial rate episode
lasting longer than five to six seconds or a rate
>
180 beats/min.
For the assessment of stroke risk and the need for
anticoagulation, the CHADS-VaSC score remains unchanged but
the stroke risk has been reclassified for women. Anticoagulation
is indicated in men with a score of 2 or more; for women it’s a
score of 3 or more. Anticoagulation is not mandated but may be
considered in men and women with respective scores of 1 or 2.
Bleeding risk scores should be considered to determine
the presence of modifiable risk factors for major bleeding
in patients taking anticoagulant therapy. A non-vitamin K
antagonist (VKA)/novel oral anticoagulant is preferred to
warfarin. Occlusion of the left atrial appendage may be
considered in patients who have a long-term contra-indication
to anticoagulation. The guideline provides recommendations
for the initiation of anticoagulation after transient ischaemic
attack or stroke and the re-initiation of anticoagulation after
intracranial bleeding.
The integrated management of AF includes symptom control,
maintenance of haemodynamic stability and the preservation of
LV function, stroke prevention and the management of CV risk
factors. Recommendations for ventricular rate control include
consideration of digoxin as a second-line therapy.
ENSURE-AF
23
examined the use of the factor Xa inhibitor
(edoxaban) versus enoxaparin/warfarin-VKA in electrical
cardioversion of non-valvular AF in 2 199 patients with and
without transoesophageal echocardiography (TEE). The average
CHADS-VaSC score was 2.6. The procedure was undertaken
with a delay of two and 23 days, respectively, depending on
whether or not patients had undergone TEE. There was a very
low event rate following cardioversion with a 50–60% reduction
in events with edoxaban and no increase in bleeding.
Cumulative event rate
1.0
0.8
0.6
0.4
0.2
0.0
0 1 2 3 4 5 6 7 8
560 540 517 438 344 248 169 88 12
556 540 526 451 358 272 186 107 17
Years
Controls
ICD
120 died in the ICD group and 131 in the control group
Hazard ratio = 0.87 (0.68 – 1.12)
p
= 0.28
Controls
ICD
Fig 2.
Primary outcome – all-cause mortality

















