
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 6, November/December 2016
AFRICA
393
WCH affects 30–40% of the hypertensive population.
Patients with WCH have a metabolic profile similar to that of
hypertensive patients. Their baseline blood pressure is marginally
higher than that of the normotensive population. The WCH
group has a higher incidence of increased pulse pressure and left
ventricular hypertrophy and a higher 10-year risk of developing
established hypertension and diabetes. The prognosis of WCH
is intermediate between normotensive and hypertensive patients
with a higher incidence of CV events. There are no therapeutic
strategies proven to be effective in WCH.
McManus and Sheppard evaluated the application of
multiple serial office blood pressure readings to reasonably
predict out-of-hospital blood pressure levels. Their data from
the PROOF blood pressure study support the value of obtaining
ambulatory blood pressure recordings in patients with an office
blood pressure of 130/80 to 144/89 mmHg, therefore requiring
ambulatory blood pressure recordings in 58% of patients.
2
They
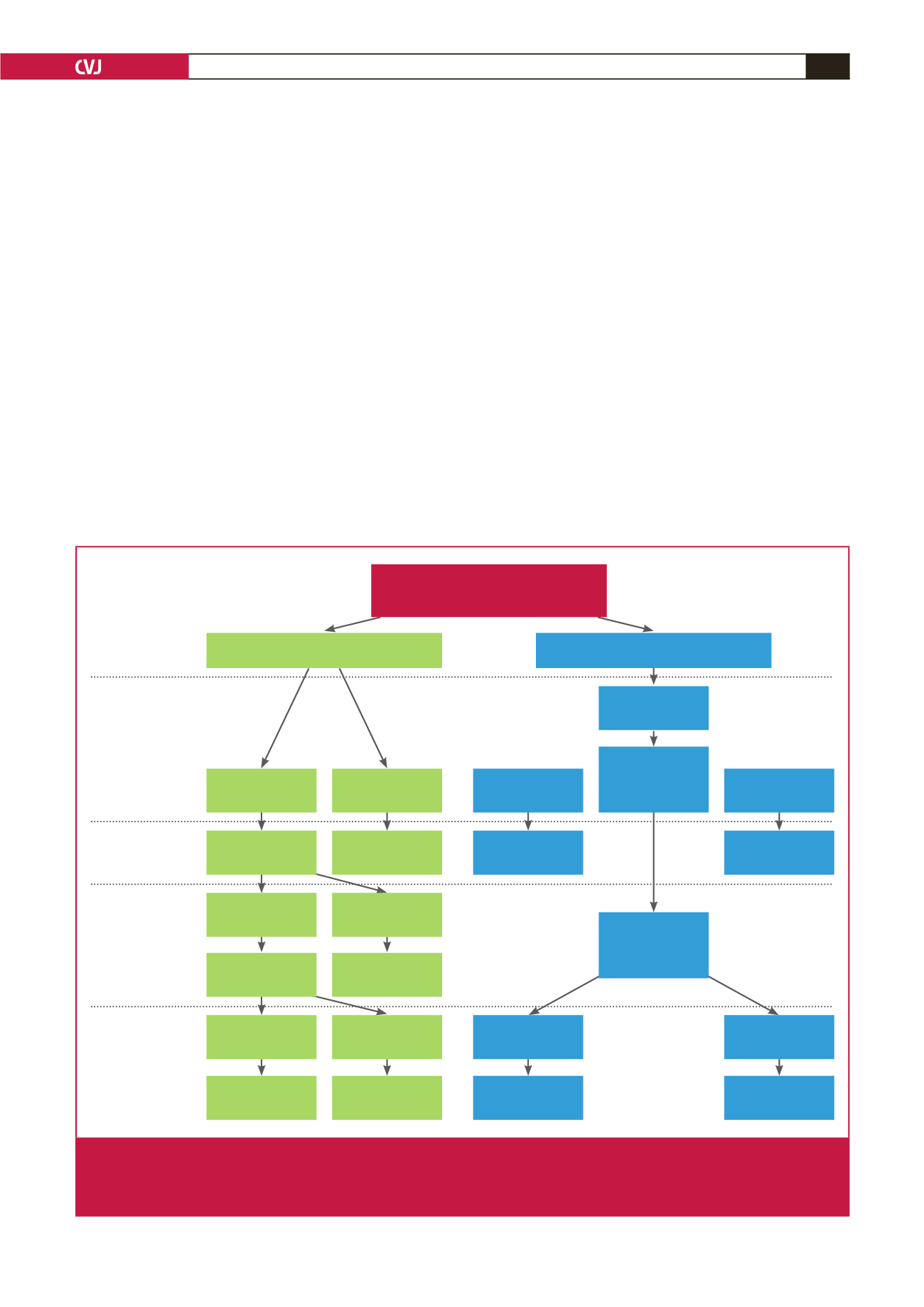
have published an algorithm for calculating home blood pressure
(https://sentry.phc.ox.ac.uk/proof-bp)(Fig. 1).
Kario from Japan pointed out that central aortic pressure is
a further component to be considered in blood pressure control.
It is best controlled with an angiotensin converting enzyme
inhibitor (ACE-I) or angiotensin receptor blocker (ARB) and
not with beta-blockade. Diurnal variation in blood pressure
and aortic stiffness are other aspects receiving attention. He
commented that when combined with an ARB (olmesartan),
hydrochlorothiazide is superior to calcium channel blockade for
the control of nocturnal hypertension.
A lunchtime symposium was devoted to the underuse of
mineralocorticoid antagonists (MRAs), namely spironolactone
and eplerenone, in both hypertension and heart failure. Both have
proven benefits in improving blood pressure control in resistant
hypertension
3
and patient survival in heart failure. Hypertension
is controlled best at a serum potassium level of around 4.5
mmol/l, but concerns about the development of hyperkalaemia
result in avoiding appropriate prescription or under-dosing of
MRAs. The survival benefit for heart failure patients is not
eliminated in those who develop hyperkalaemia. However, the
detection of a high potassium level most often leads to the
discontinuation of the whole spectrum of renin–angiotensin–
aldosterone system (RAAS) inhibitors and a consequent loss
of efficacy. Hyperkalaemia may be controlled in the short term
Offer treatment
Calculate adjusted
clinic BP
Blood pressure
measurement
strategy
Initial management
decision
Additional blood
pressure monitoring
or management
Final management
decision
Clinic blood
pressure screening
Ambulatory BP monitoring
PROOF-BP algorithm
Clinic BP
>140/90 mmHg
Adjusted clinic BP
<130/80 mmHg
Measure again in
5 years
Sustained clinic BP
>140/90 mmHg
Send for amulatory
BP monitoring
Ambulatory BP
>135/85 mmHg
Ambulatory BP
>135/85 mmHg
Offer treatment
Clinic BP
<140/90 mmHg
Adjusted clinic
BP from 130/80 –
144/89 mmHg
Adjusted clinic BP
>130/80 mmHg
Measure again in
5 years
Offer treatment
Send for
ambulatory BP
monitoring
Subsequent clinic
BP <140/90 mmHg
Measure again in
5 years
Ambulatory BP
<135/85 mmHg
Ambulatory BP
<135/85 mmHg
Measure again in
5 years
Measure again in
5 years
General population
Clinic BP 120/70 – 250/130 mmHg
Repeat clinic
measurment
Fig 1.
Algorithm for using the Predicting Out-of-Office Blood Pressure in clinic tool (PROOF-BP) prediction model to triage
patients for out-of-office blood pressure monitoring. Existing strategies are based on the hypertension diagnostic path-
way specified by the US Preventive Services Task Force and the National Institute for Health and Care Excellence. BP
indicates blood pressure. Source:
Hypertension
2016;
67
(5): 941–950.

















