
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 6, November/December 2016
e2
AFRICA
junction (Fig. 1A). Posterior to the aorta, turbulent flow of the
CF originating from the left coronary system was detected (Fig.
1B). The Qp/Qs was 1.7.
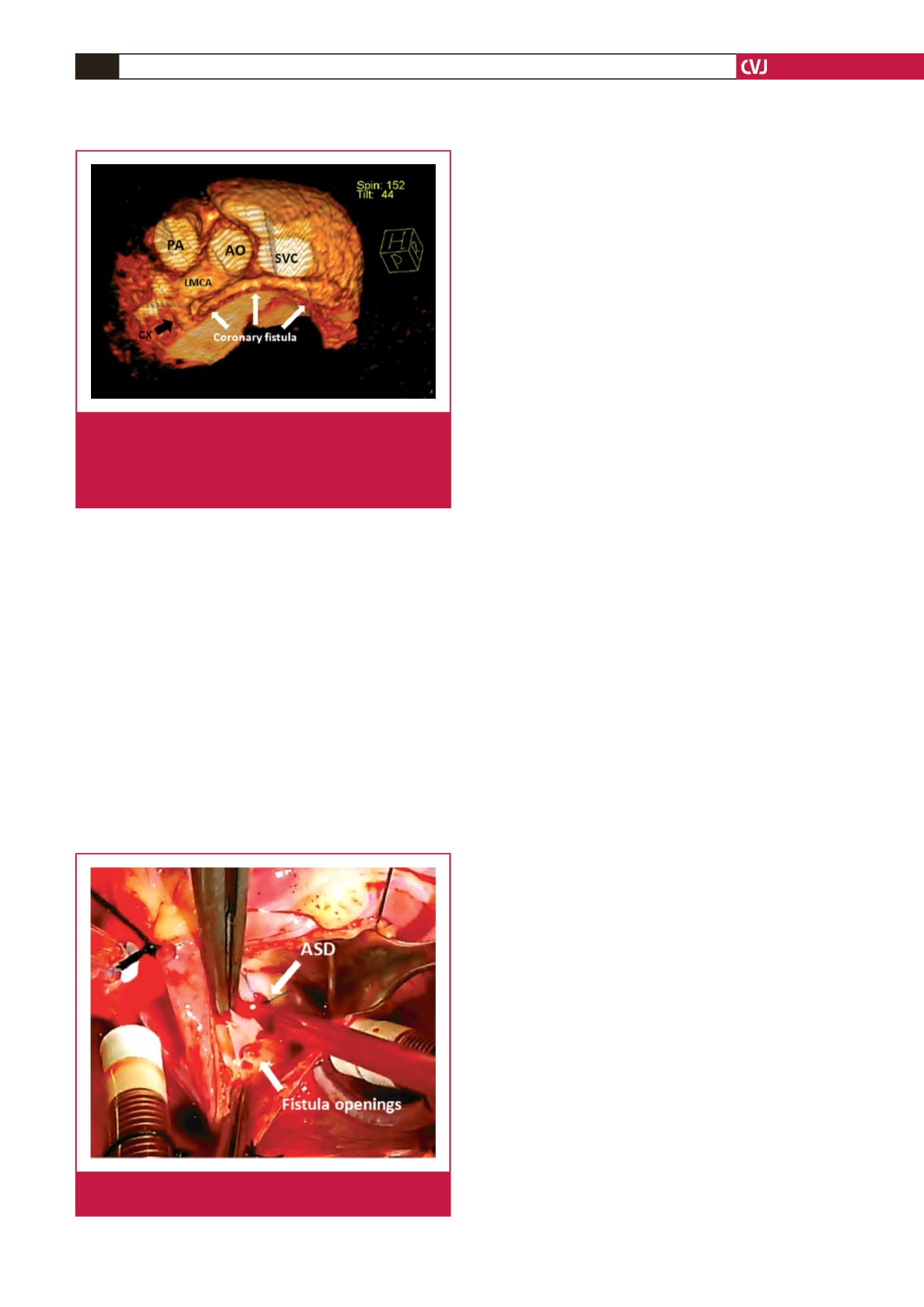
In contrast-enhanced computed tomography, the left main
and circumflex coronary arteries were dilated (6 and 4.5 mm,
respectively). The CF originated from the proximal Cx and
coursed posterior to the aorta before draining into the RA (Fig.
2). Because of the small size of the patient, percutaneous closure
of both the ASD and CF was not appropriate therefore surgical
closure was planned.
After a median sternotomy and pericardiotomy, the CF was
located adjacent to the posterior part of the superior cavo-atrial
junction. Under cardiopulmonary bypass (CPB), the aorta was
cross-clamped and cardiac electromechanical quiescence was
established. Through a right atriotomy, the secundum ASD was
primarily closed.
It was detected under cardioplegic wash-out that the opening
of the CF was located inferior to the cavo-atrial junction and
it had multiple openings, which were connected with a loose
membrane (Fig. 3). Following the primary closure of the
openings from within the RA, the connection was checked with a
second cardioplegic wash-out. Because of the loose membranous
connection between the openings and to ensure that the fistulous
connection was separated, the fistula was ligated outwardly,
close to the opening of the RA. After weaning from CPB, no
electrocardiographic changes indicative of myocardial ischaemia
occurred.
The postoperative course was uneventful. In postoperative
echocardiography, the atrial septum was intact and no turbulent
flow in the right atrium was detected. Aspirin was given for
three months. At the six-month follow-up visit, he was found
to have gained weight (12 kg). Additionally, no turbulent flow
within the atrium or posterior to the aorta was detected in
echocardiographic evaluation.
Discussion
As the use of selective coronary angiography became widespread,
recognition of a CF has been improving since the 1950s.
1
Sercelik
et al
. found the incidence of congenital CFs in the Turkish
population was 0.08%.
4
Among 286 cases with CF, the source
of the CF was the right coronary artery in 56% and the left
coronary system in 36% of cases.
In the literature, while the Cx was the least common source
of a CF, the right heart chambers were the most common
location of drainage.
1-7
Although spontaneous closure has been
demonstrated, either surgical or interventional closure of the
CF was recommended during childhood, even though they
were asymptomatic, because of the risks that can occur during
adulthood, including myocardial ischaemia, endocarditis and the
complications of long-standing left-to-right shunt.
2,5,7
Contrary to our case, nine of 10 CFs were asymptomatic in
an evaluation of CFs in paediatric cases, and surgical ligation
under CPB support without application of an aortic cross-
clamp was performed in four cases.
5
According to Sakakibara
et al
.,
3
our CF was type A in which ligation of the CF distal to
the origin without CPB was recommended. Because the patient
was symptomatic and due to the associated ASD, of which
percutaneous closure was not feasible, we implemented ASD
closure under CPB, suture closure of the atrial opening of the
fistula from within the RA, and ligation of the CF outwardly,
close to the connection with the RA.
Conclusion
In our opinion, based on the clinical presentation and coexistent
cardiac pathology, the choice of therapeutic management
strategy should be individualised. Because of the possibility of
the development of complications in the future, we successfully
operated on a symptomatic paediatric case in whom the CF was
incidentally diagnosed in association with an ASD.
References
1.
Lowe JE, Oldham HN, Jr., Sabiston DC, Jr. Surgical management of
congenital coronary artery fistulas.
Ann Surg
1981;
194
: 373–380.
Fig. 2.
Three-dimensional reconstructed computed tomo-
graphic view demonstrating the trajectory of the coro-
nary fistula. Note the dilated left main and circumflex
coronary arteries. AO: aorta, LMCA: left main coronary
artery, PA: pulmonary artery, SVC: superior vena cava.
Fig 3.
Surgeon’s view revealing the multiple openings of the
coronary fistula. ASD: atrial septal defect.

















