
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 4, July/August 2017
e10
AFRICA
anti-anginal therapy, including intravenous nitroglycerin and
morphine sulfate. In addition, we reversed the effects of heparin
with protamine sulfate.
On day three of the follow up, cardiac computed tomography
revealed thickening of the lateral wall of the myocardium, a
radiolucent centre without contrast dye, and bilateral pleural
effusions with no pericardial effusion (Fig. 2B, C). The patient
developed transient atrial fibrillation and dyspnoea on the third
day. Sinus rhythm was achieved with intravenous amiodarone,
and the heart failure symptoms and findings disappeared with
diuretics.
The patient did not complain of chest pain or arrhythmia
after the third day, and she was discharged on the sixth day of
follow up. There was no haematoma in the lateral wall of the
left ventricle but this part of the left ventricle was akinetic in the
control echocardiography after 45 days.
Discussion
DIH can occur as a complication of myocardial infarction, PCI
and cardiac surgery.
1
Prediction and diagnosis of DIH is very
difficult after PCI and cardiac surgery. There are a few cases of
DIH after PCI reported in the literature.
2
Continued leakage of blood from the coronary artery after
any kind of perforation and avulsion of the vessel can lead to
dissection of the myocardium and it is characterised by dissection
between the spiral planes of heart muscle, including laminated
thrombi, myocytes and fibrous tissue.
2
Self-propagation of the
haematoma leads to more expansion, and it can be complicated
by myocardial wall rupture.
3
Patients with previous cardiac surgery may have a self-
limiting DIH because of pericardial adhesions to the epicardium.
Therefore, these patients may be protected from myocardial
rupture.
4,5
Since it is a rare situation, management of DIH is challenging
in evidence-based medicine. Conservative management of DIH
is associated with a mortality rate as high as 90 to 100%.
2
Management strategies depend on the location and/or extent of
the DIH.
Left ventricular apical location of the DIH has higher
spontaneous reabsorption rates so conservative management is
preferable for this position. Evacuation of the DIH and surgical
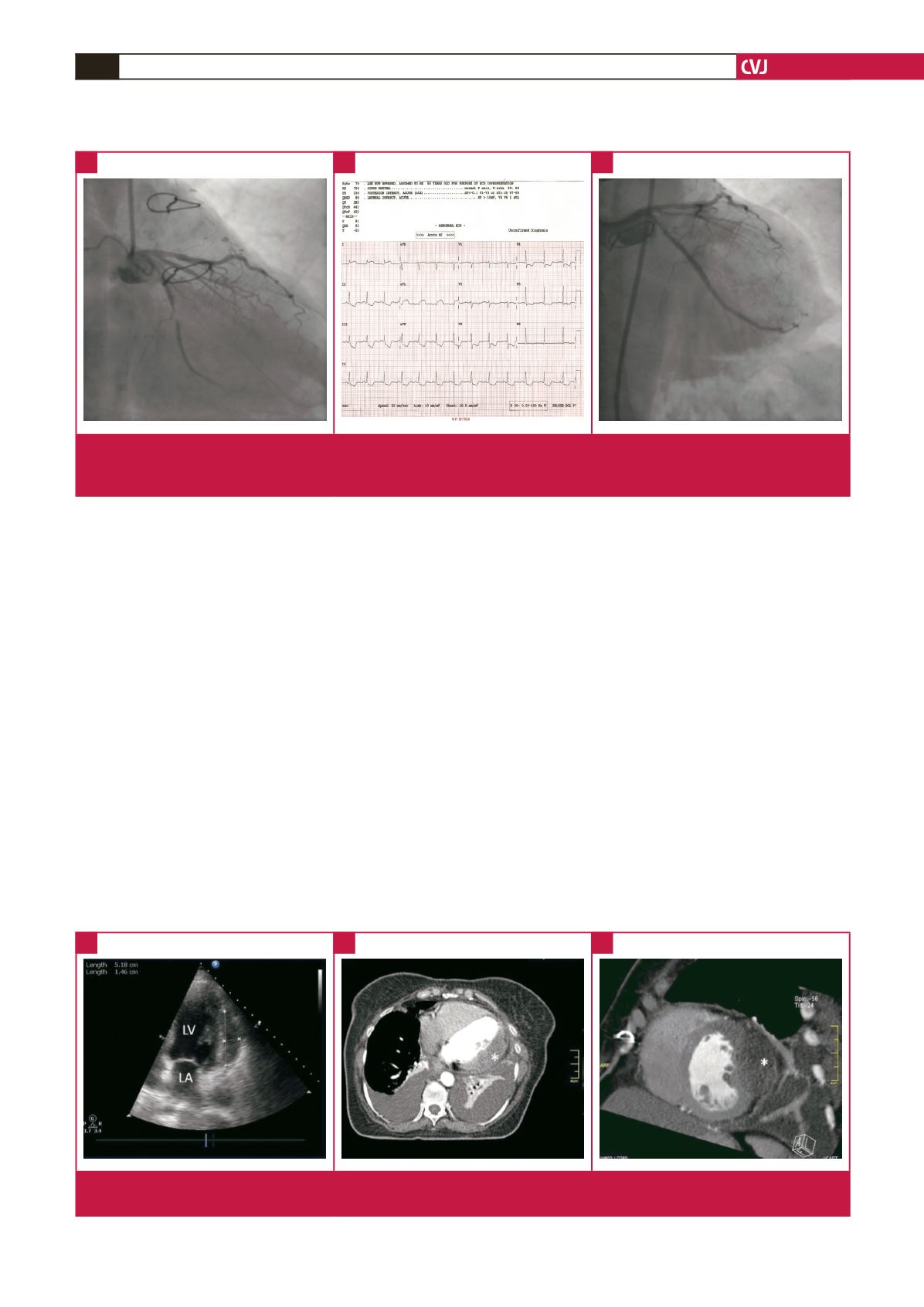
Fig. 2.
A. Transthoracic echocardiography. B, C. Axial and sagittal computed tomography sections of the heart. Intra-myocardial
haematoma is seen in both echocardiography and computed tomography (asterisk). LV, left ventricle; LA, left atrium.
A
B
C
Fig. 1.
A. Coronary angiography before PCI. B. ECG after PCI. C. Control angiography. Significant stenosis is seen in the circum-
flex artery (A) and there is no contrast dye leakage in the control angiography (C) in the right caudal position. There is ST
segment elevation in D1 and aVL deviations, suggesting a new-onset acute coronary syndrome.
A
B
C

















