
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 1, January/February 2018
14
AFRICA
performed during the warming phase after ascending aortic tube
graft implantation. After cardiopulmonary bypass (CPB) was
terminated, the surgery was completed with haemostatic control.
Statistical analysis
Statistical assessments were performed using Microsoft Excel
software. All numerical data are presented as mean
±
standard
error, while categorical variables are presented as percentages.
Results
The mean age of the patient group was 58
±
2 years and 54.8% of
the study population was male. Demographic characteristics and
pre-operative data of the study patients are shown in Table 1.
Aortic root replacement was performed in 14 patients. Four
received surgical valvular repair, and a total of 18 patients
underwent aortic valve replacement, including a modified Bentall
procedure with flanged grafts in 10 patients (Table 2).
The mean CPB and cross-clamp times were 80
±
18 and 53
±
18 minutes, respectively. The mean postoperative drainage
volume was 375
±
75 ml. The mean transfusion rate of
erythrocyte suspension was 1.1
±
0.3 units (Table 3). No patient
required revision surgery and the average duration of hospital
stay was 7.9
±
1.4 days.
Discussion
Among cardiac operations, aortic surgery is generally associated
with higher volumes of blood loss due to a number of factors,
including thinned, atherosclerotic, calcific or fragile aortic
tissue, and also due to re-implantation of the coronary arteries.
Following an anastomosis, bleeding occurring posteriorly poses
a particular challenge since it may require re-initiation of CPB.
Different methods have been reported to reduce the risk
of postoperative bleeding in these patients.
1-4
In our practice,
autogenous aortic tissue is generally used to reduce the risk of
bleeding based on the advantage of tissue continuity. Also, easier
control of bleeding with additional sutures on the native aortic
tissue represents an additional benefit of this approach. We
therefore perform anastomosis after obtaining double-layered
aortic tissue with eversion of the autogenous aorta.
Among our 42 patients undergoing ascending aorta
replacement using this technique, no complications occurred and
there were no cases requiring re-operation. The average drainage
volume was 375 ml. No cases of postoperative morbidity/
mortality associated with pseudo-aneurysms, complications due
to the use of foreign materials, or bleeding were recorded.
Prolonged CPB, hypothermia and administration of heparin
are associated with an increased risk of postoperative bleeding
in patients undergoing cardiac surgery,
6
leading to increased
requirement for transfusion, with a subsequent increase in the
risk of infection, anaphylaxis and renal/pulmonary injury.
6
With
this technique as described above, an average of 1.1
±
0.3 units
of erythrocyte suspension were transfused in approximately
two-thirds of our patients.
Pseudo-aneurysms may arise at the suture line after ascending
aorta graft replacement, or infections may cause dehiscence at
the suture line,
7-10
elevating the risk of mortality and need for
re-operation. Higuchi
et al
.
11
reported lower risk of bleeding
using continuous sutures for anastomosis after the inclusion of a
7-cm segment of Dacron tube graft, folded with three sutures to
achieve a double-layered structure. However, this approach may
be expected to increase the early risk of thrombosis formation
in the graft as well as embolic risk, since the contact surface
between the synthetic graft material and the aorta is increased.
On the other hand, the method described above, involving
eversion of the autogenous aortic tissue would not only reduce
the amount of intra-luminal tissue, but would also exploit the
advantage of using autogenous tissue. Use of as much viable
tissue as possible during graft replacement may also hasten the
postoperative healing process at the suture lines, reducing the
risk of pseudo-aneurysm.
Ohata
et al
.
3
reported the use of a graft interposition
technique in which the aortic tissue is folded inside, leaving a felt
band in the outer layer. In this technique, continuous prolene
sutures were preferred, and in contrast with our approach, the
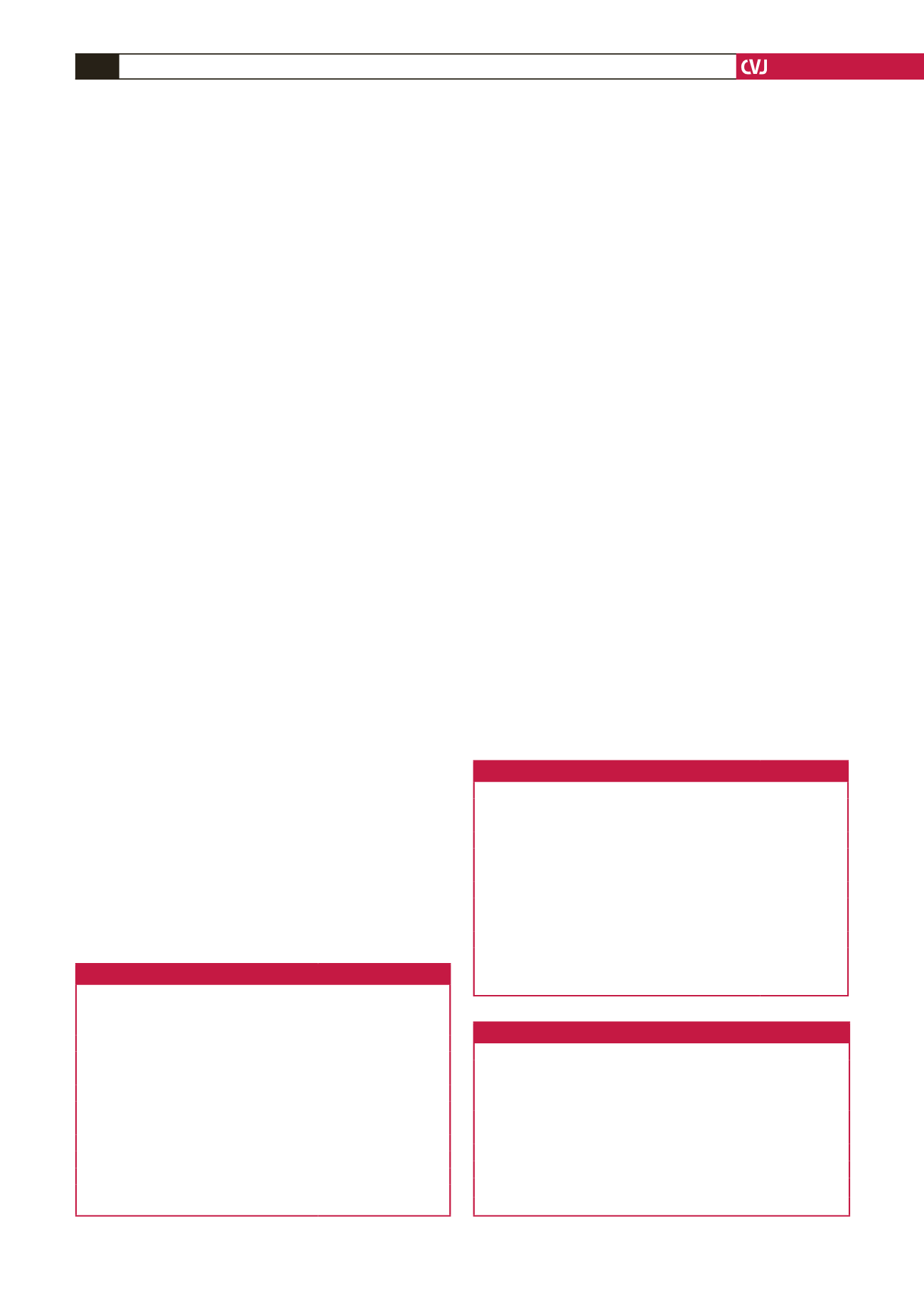
Table 1. Pre-operative demographical data of the patients
Variable
Value
Age (mean
±
SD)
58.2
±
13.9
Male,
n
(%)
23 (54.8)
Hypertension,
n
(%)
21 (50)
Diabetes,
n
(%)
1 (2.3)
Chronic renal failure,
n
(%)
0 (0)
COPD,
n
(%)
6 (14.2)
Coronary artery disease,
n
(%)
8 (19)
History of CVA,
n
(%)
2 (4.8)
Re-operation,
n
(%)
1 (2.3)
Pre-operative EF (%) (mean
±
SD)
58.2
±
13.8
Aortic insufficiency,
n
(%)
22 (52.4)
SD: standard deviation, EF: ejection fraction, COPD: chronic obstructive
pulmonary disease, CVA: cerebrovascular accident.
Table 2. Surgical procedures
Variable
Value
Ascending aortic repair without valve procedure
20
Ascending aortic repair with valve procedure
22
Bentall procedure
10
David operation
4
Separated graft interposition
8
Concomitant surgical intervention
AVR
18
CABG
8
Mitral valve repair
1
ASD repair
1
AVR: aortic valve replacement, CABG: coronary artery bypass grafting, ASD:
atrial septal defect.
Table 3. Surgical findings
Variable
Value
Duration of cross clamp, min (mean
±
SD)
52.9
±
17.7
Duration of cardiopulmonary bypass, min (mean
±
SD)
79.8
±
18.5
Drainage, ml (mean
±
SD)
375
±
75
Revision,
n
0
Erythrocyte replacement, units (mean
±
SD)
1.1
±
0.3
Duration of intubation, hours (mean
±
SD)
5.3
±
1.1
Postoperative EF, % (mean
±
SD)
54.8
±
6.3
Duration of hospitalisation, days (mean
±
SD)
7.9
±
1.4
SD: standard deviation, EF: ejection fraction.

















