
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 1, January/February 2018
e10
AFRICA
favouring missed diagnosis of AAD were walk-in patients,
anterior chest pain, severe or worst-ever pain and widened
mediastinum, with walk-in mode of admission being the single
strongest predictor of misdiagnosis.
8
Diagnostic imaging studies are pivotal in confirming the
diagnosis and classifying the extent of the dissection using either
DeBakey (I, II and III) or Standford (A or B) classifications.
AAD involving the ascending aorta (Standford type A) is a
surgical emergency requiring swift repair of the aortic root
or reconstruction of the ascending aorta and arch to improve
prognosis, whereas dissections involving the descending aorta
(Standford type B) are treated medically with the following
surgical indications: propagation of the dissection, intractable
pain or poor organ perfusion.
3,12
Case report
A 53-year-old sub-Saharan African man with poorly controlled
hypertension was referred to the cardiac intensive care unit
(CICU) by his cardiologist for themanagement of a sudden-onset,
severe and intractable retrosternal chest pain of approximately
50 hours’ duration. The pain was tearing in character, radiating
to the back and lumbar regions, non-positional and associated
with shortness of breath and headache.
The electrocardiogram (ECG), done three hours after
the onset of pain, showed sinus rhythm and non-specific
repolarisation changes (flattened or inverted T waves in leads I,
aVL and V3–V6). Although ECG changes were suggestive of left
ventricular strain, the presence of chest pain and a mildly raised
troponin level (0.11
µ
g/ml) favoured myocardial infarction,
and the patient was started on low-molecular weight heparin
(LMWH) at a therapeutic dose, aspirin and nitrates.
Persistence of the pain after initial therapy prompted referral
to our centre. On examination, he was anxious, dyspnoeic
(NYHA functional class III with a respiratory rate of 28 breaths/
min) and diaphoretic. His temperature was 36.9°C, heart rate
was 79 beats/min, and blood pressure was 187/73 mmHg in
the right arm and 145/56 mmHg in the left arm. Physical
examination showed a systolic murmur (grade 3/6) in the aortic
area, which radiated to the left carotid, but there were no signs of
heart failure. The neurological examination was unremarkable.
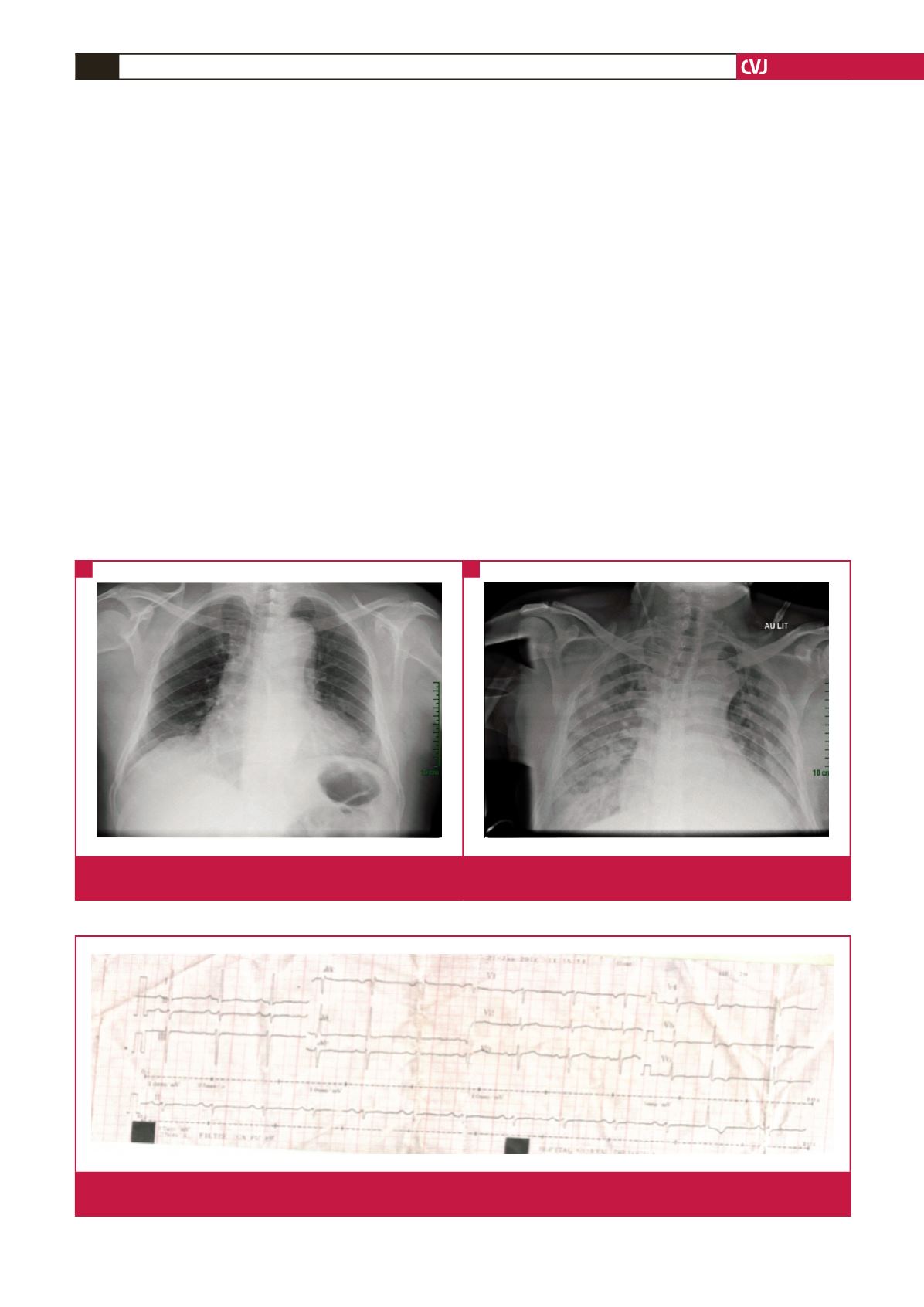
Chest X-ray (Fig. 1A) showed enlargement of themediastinum
Fig. 1.
Anterior–posterior chest X-ray. A: At presentation showing enlargement of the mediastinum. B: On day 11 of hospitalisation
showing bilateral interstitial heterogeneous opacities.
A
B
Fig. 2.
ECG at presentation showing non-specific ST-segment changes consistent with sub-epicardial ischaemia in the inferior and
apico-lateral leads.

















