
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 1, January/February 2018
AFRICA
e7
urea nitrogen (BUN)
=
17 mg/dl, creatinine
=
0.94 mg/dl, creatine
phosphokinase (CK)
=
847 U/l, CK-MB
=
58 U/l. He was moved
to the cardiac surgery department. During this first postoperative
day, the patient was stable, awake and oriented. No signs of
haemodynamic instability or cardiac dysrhythmias were seen.
The second day after CABG, the overall condition of the
patient was good but he had difficulty moving his lower limbs.
Neurological consultation was done and the cranial nerves were
found to be intact, cerebellar tests and sensory examinations
were normal, muscle strength of the lower limbs was 3/5 and
symmetric and plantar reflexes were double flexor.
On the third postoperative day, the overall condition of the
patient was good but he still had difficulty moving the lower
limbs. Progressive paraparesis developed and the muscle strength
and deep tendon reflexes (DTRs) began to decrease gradually.
Paraparesis progressed and muscle strength decreased from 4/5
to 3/5 and then to 2/5. In the evening, severe weakness of the
lower and upper limbs developed, absence of DTRs, no plantar
reflexes, and muscle strength was 1/5 on the left and 0/5 on the
right side. That night the patient presented with respiratory
failure; he was intubated and moved to the ICU.
On the fourth day, the patient was haemodynamically
stable and he was transferred to the radiology laboratory in
order to undergo magnetic resonance imaging (MRI). During
the MRI examination, the patient experienced an episode of
ventricular fibrillation and cardiac arrest. He was resuscitated
after 20 minutes of cardiopulmonary resuscitation and two
defibrillations. He was in haemodynamic instability and received
high doses of dobutamine, norepinephrine and adrenaline.
The laboratory findings were: creatinine
=
3.0 mg/dl, urea
111 mg/dl, aspartate transaminase (AST) 1 000 U/l, alanine
transaminase (ALT) 6182, LDH 9 119 U/l, CK 3 915 U/l,
CK-MB 315 U/l, troponin 10 000 ng/ml. The echocardiogram
findings were left atrium 39 mm, telo diastolic volume of the left
ventricle 50 mm, the left ventricle showed diffuse hypokinesis
and akinesis, with a LVEF of 25%, and pulmonary artery
systolic pressure was 40–45 mmHg.
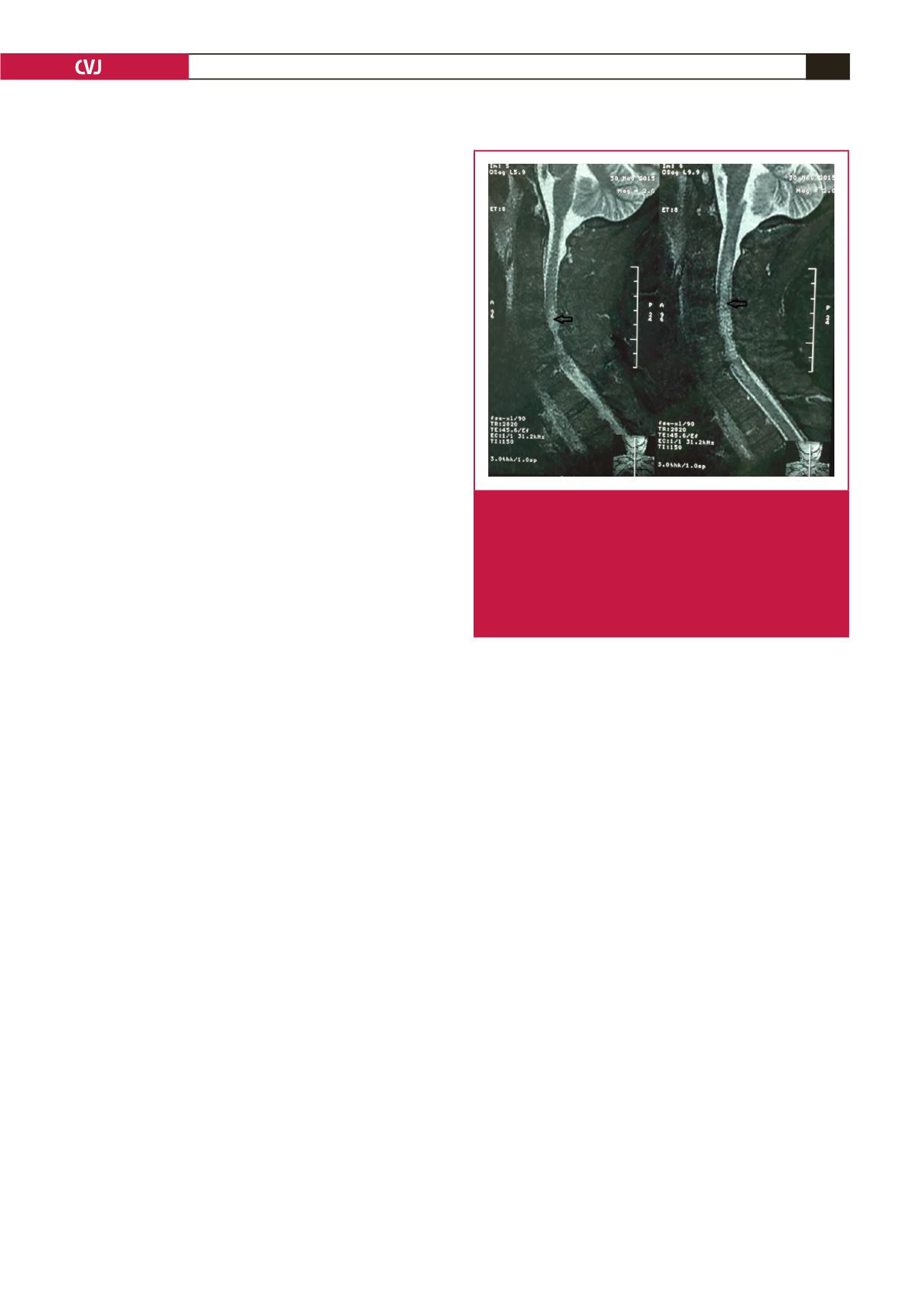
The MRI report showed at the level of the fifth and sixth
cervical vertebrae that there were posterior osteophytes and
circular degeneration of the annulus fibrosis with high-grade
stenosis and compressive phenomena in the spinal cord. From
the second to the sixth cervical vertebrae, there was a pathological
zone and oedema due to myelopathy and ischaemia (Fig. 1).
On the sixth day after surgery, the patient was better and was
haemodynamically supported with low-dose norepinephrine.
However he presented manifestations of post-cardiac arrest
brain injury such as coma, seizures and myoclonus. He died 10
days after surgery due to septic shock.
Discussion
Neurological complications after cardiac surgery may occur in
the post-operative period. Stroke and transient ischaemic attack
are major adverse cardiac events following CABG and markedly
reduce patient short- and long-term survival rates. The five-year
rate of stroke was significantly higher after CABG than after
percutaneous coronary intervention in patients with diabetes and
multi-vessel coronary artery disease.
2
Previous studies comparing
surgical outcomes of patients undergoing conventional on-pump
CABG with cardiopulmonary bypass versus patients undergoing
off-pump CABG mostly focused on low-risk patients, for
instance, relatively young patients with preserved left ventricular
function and without systemic co-morbidity.
The causes of these neurological complications are hypoxia,
metabolic abnormalities, emboli or haemorrhage. These
complications can be divided into two types: type 1 (3%) includes
major focal deficit and stupor or coma; type 2 (3%) includes
intellectual dysfunction. These complications are associated with
increased mortality rates, prolonged ICU stay and decreased
long-term survival rates.
1-7
Risk factors for neurological complications in cardiac surgery
are haemodynamic instability, diabetes mellitus, advanced
age, complex procedures, prolonged CPB (
>
two hours),
previous stroke, hypertension, hyperglycaemia, hyperthermia,
hypoxaemia, aortic atheromatosis and peripheral vascular
disease.
1,2,5
Mechanisms and factors causing neurological lesions
are embolisation and hypoperfusion, and influencing factors
are aortic atheroma plaque, cerebrovascular disease, altered
cerebral autoregulation, hypotension, intracardiac debris air,
venous obstruction on bypass, CPB circuit surface, cerebral
hyperthermia and hypoxia.
In our case, the differential diagnoses were cerebrovascular
accident or lacunar infarct (internal capsular region) – embolic or
haemorrhagic, spinal cord ischaemia and infarct (due to embolic
insult or hypoperfusion), acute inflammatory demyelinating
polyradiculoneuropathy or critically ill polyneuropathy,
peripheral nervous injury, peripheral vascular disease and spinal
cord ischaemia. In spinal cord ischaemic stroke, neurological
deficits may occur without pain, however, most (
>
80%) are
painful and this is an interesting difference from cerebral
infarction, which is usually not painful. Depending on the level
Fig. 1.
At the level of the fifth and sixth cervical vertebrae,
posterior osteophytes and circular degeneration of
the annulus fibrosis with high-grade stenosis and
compressive phenomena in the spinal cord can be
seen. From the second to the sixth cervical level, a
pathological zone (white area into the grey zone) and
oedema due to myelopathy and ischaemia (arrows)
can be seen.

















