
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 3, May/June 2019
154
AFRICA
the ASI diminished significantly; however it was significantly
higher in group B than in the control group at the six-month
follow-up assessment (
p
<
0.05) (Table 4).
The explanation of these findings is that since the PDA
is typically connected with a hyperdynamic status and there
is a vascular shunt between the aorta and pulmonary artery,
congenital aortic changes occur (aortic stiffness). Additionally,
shunt injuries may be related to a provocative inflammatory
process, and endothelial malfunction may hasten the ageing
of vessels, particularly the aorta.
7
Haemodynamic and oxygen
saturation changes (nocturnal hypoxaemia) may be the
fundamental components of aortic stiffness in shunt injuries
because of increased PAP, notwithstanding the inflammation
and endothelial disruption.
8
Our study additionally discovered that patients in group B
had a higher ASI than those in group A preceding closure (
p
<
0.05). After closure, the ASI diminished significantly (
p
<
0.05);
however the ASI was higher in group B than in group A at the
six-month follow-up assessment (
p
<
0.05) (Table 2). There was
no notable difference between patients in group A and B with
regard to the PDA size (
p
=
0.1). This was in accordance with
previously published information,
9
which demonstrated that
ageing is related to expanding aortic stiffness as evaluated by
both aortic pulse wave velocity and local aortic dispensability.
In group A, our study indicated that patients with PDA had
significantly lower LVEF than the control group before closure
(
p
<
0.05). After closure, the LVEF was significantly enhanced (
p
<
0.05), and there was no notable distinction between the patient
groups and the control group (
p
=
0.6) at the six-month follow-up
assessment (
p
<
0.6) (Table 3).
In group B, patients with PDA had a significantly lower
LVEF than the control group before closure (
p
<
0.05). After
closure, the LVEF was significantly enhanced and there was a
significant difference between the patient groups and the control
group at the six-month follow-up assessment (
p
<
0.05) (Table 4).
There was a significant distinction between the patient groups
and the control group with regard to the LVEDD and LVESD
before closure (
p
<
0.05). After closure, the LVEDD decreased (
p
<
0.05); however, it was somewhat higher in the patient groups
than in the control group at the six-month follow-up assessment
(
p
<
0.05) (Table 4). The explanation of these findings is that the
change in heart function in both groups after PDA closure was
clarified by interruption of the left-to-right shunt, which limited
the left ventricular volume overload.
10
Our discoveries are in agreement with previous studies that
demonstrated that subjects with PDA had higher LV end-systolic
volume index and LV end-diastolic volume index, a decreased
LVEF, and a higher BNP level compared with those in the
control group. These progressions are reported and settled over
a six-month follow-up period after percutaneous PDA closure.
11
Our findings with regard to diastolic physiological changes
demonstrated that there was a diastolic physiological weakness
in patients with PDA. Park
10
discovered a weakened pattern in
the early change of diastolic capacity after the development of
a restrictive pattern. In this study, we revealed that patients with
PDA had a significantly higher E/Ea ratio (ratio of early mitral
flow velocity to early mitral annular velocity) than the control
group before closure (
p
<
0.05). After closure, the E/Ea ratio was
enhanced (
p
<
0.05) and higher than that in the control group at
the six-month follow-up assessment (
p
<
0.05) (Tables 3, 4).
BNP is discharged by the ventricular myocytes in light of the
LV volume overload, which is associated with a large left-to-right
shunt.
12
The BNP hormone could be developed as a marker for
heart failure and treatment assessment.
13
In this study, we discovered that BNP level was significantly
higher in children with PDA in both groups prior to closure than
in control subjects (
p
<
0.05), while levels diminished significantly
six months after closure (
p
<
0.05), approaching non-significance
compared with that in the control group (
p
>
0.05) (Tables 3,
4). We discovered that the BNP level was significantly higher in
patients in group B than in those in group A preceding closure
(
p
<
0.05). After closure, there was no substantial distinction
between groups with regard to BNP levels (
p
=
0.3) (Table 2).
Eerola
et al
.
11
found that the BNP level diminished significantly
from 141 (31–974) ng/l to 79 (21–480) ng/l in six months after
PDA closure. They likewise found that the BNP level of children
with PDA was significantly different compared to that in healthy
children.
11
Therefore the BNP level could be utilised as a marker
of heart dilatation.
In our patients with PDA, a significant connection was found
between serum levels of BNP and the aortic stiffness index.
This was consistent with the results of a previous review
14
that
discovered the relationship between BNP level and ASI.
Plasma levels of BNP have been shown to relate to systolic
pressure in the right ventricle (RV) in children with volume
overload of the RV.
15
Plasma levels of BNP have been associated
with right atrial and ventricular pressures in a child populace
comprising various loading conditions and a wide age range.
16
The results after closure of an expansive PDA are dependent
on the age at the time of repair and the presence of pre-operative
pulmonary vascular disease.
17
Age is a critical indicator of
pulmonary vascular disease. The consensus is that children under
one year of age will probably not have irreversible PAH, and
most concur that irreversibility begins at age one to two years.
This speculation has a few impediments as the pathogenesis
of irreversible PAH and its movement is multifactorial and
inconsistent.
Blount
et al
.
18
demonstrated that a PDA may have a greater
impact on the pulmonary flow than on a ventricular septal
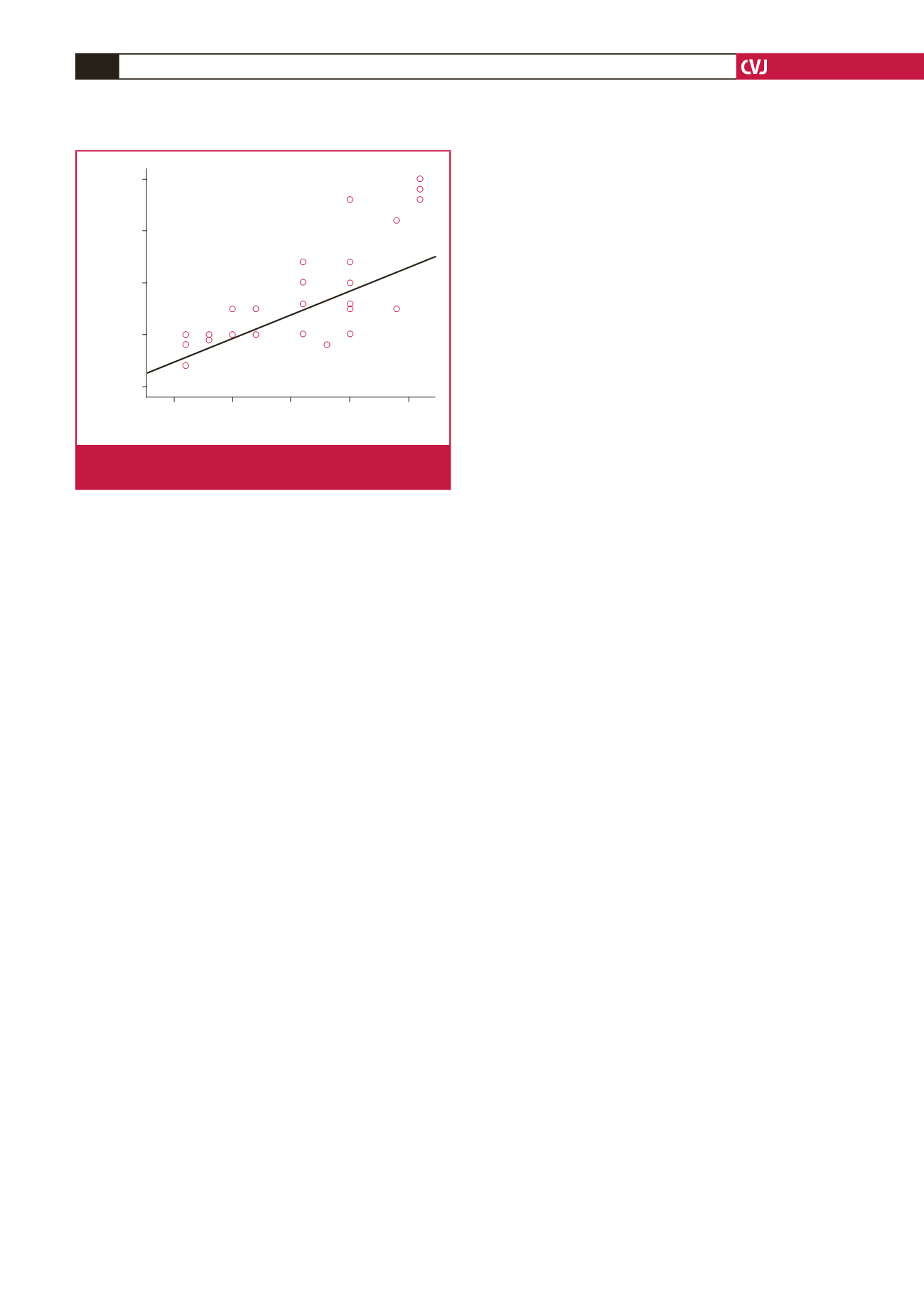
ASI
2.5
5.0
7.5
10.0
12.5
LVEDD
6.0
5.0
4.0
3.0
2.0
r
= 0.645
p
= 0.001**
Fig. 3.
A significant positive correlation is shown between the
ASI and LVEDD.

















