CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 1, January/February 2020
AFRICA
35
In premature infants, IVH was diagnosed using cranial
ultrasound before cardiac catheterisation. Furthermore, in those
infants with IVH, heparin was not given and only venous access
was used. However, when there was difficult access through
either venous or arterial access, single access was used to close the
PDA, as the ADO II AS device is deliverable both anterogradely
and retrogradely. Following angiographic assessment and if the
PDA was amenable to percutaneous closure, a device thought
to be appropriate for PDA closure was selected using the
manufacturer’s device selection guidelines.
After percutaneous ductal closure, patients received
intravenous antibiotics and would receive infective endocarditis
prophylaxis for six months. Patients had clinical and
echocardiographic follow up. Clinical follow up entailed a general
examination, including a check-up of the vascular access site for
catheterisation, pedal pulses and the rest of the cardiovascular
system. This included the detection of cardiac murmurs, aortic
regurgitation and features of congestive cardiac failure. These
are known as complications of percutaneous PDA closure
(Abbott Laboratories, St Jude Medical, St Marks, Minnesota).
The clinical follow up consultations with echocardiography were
scheduled in one day, one, three and six months, one year and
ultimately two years following PDA occlusion, using this device
as per our protocol and as suggested by the manufacturer.
Results
During the period June 2011 to June 2017, 92 patients underwent
closure of a PDA using the ADO II AS device in a single centre,
and 59 of these had a weight of less then 6 kg at the time of the
intervention. There were 15 premature infants who had a PDAwith
failed medical therapy with either oral ibuprofen or intravenous
paracetamol and remained with an echocardiographically hsPDA
with FiO
2
requirements of
>
60%.
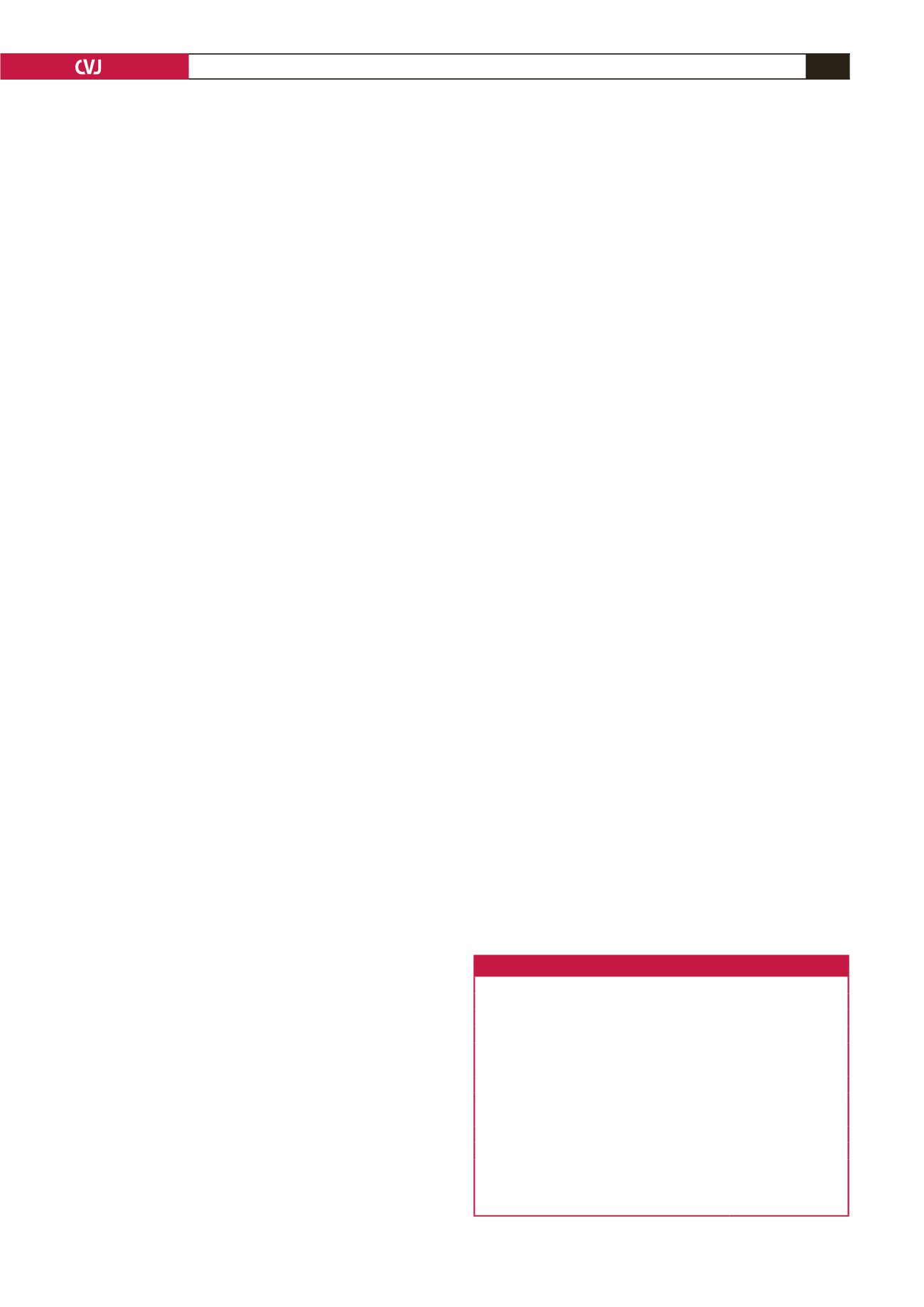
Demographic, haemodynamic and angiographic data are
presented in Table 1. There were 32 females and 27 males. The
median age of the cohort was four months (range: 23 days to
12 months). The weight ranged from 0.9 to 5.8 kg (median: 3.6
kg) in these infants. There was significant left-to-right shunting
across the PDA, with a median pulmonary-to-systemic blood
flow ratio (Qp:Qs) of 2.4 in this group. Haemodynamic studies
were performed on 96.6% of the patients (57 out of 59). The
pulmonary artery mean range was 9–47 mmHg and that of
pulmonary vascular resistance was 0.3–7.12 Wood units (Table 1).
There were 16 patients with a type A PDA (Fig. 2A, B), 15
with a type C (Fig. 2C, D), four with a type D (Fig. 2E, F), and
24 with a type E (Fig. 2G, H). There were no patients with a type
B PDA. There were no patients with a ductal diameter of
>
4 mm
across the whole cohort, as the largest ductal diameter was 3.4
mm with the median ductal length was 8.8 mm (Table 1). The
descending aortic median was 5.3 mm in the group.
The commonest devices used were the longest devices (
n
=
52; 88.1%), which included 03x06L (
n
=
12), 04x06L (
n
=
16)
or 05x06L (
n
=
24) devices. These were chosen according to
manufacturer guidelines.
The device was deployed through the pulmonic side in 41
patients and retrogradely in 18. Difficulty in finding either
venous or arterial access dictated the delivery approach of the
device since the device could be delivered either in a prograde
(anterograde) or retrograde fashion.
There was immediate ductal closure in 43 patients and closure
on day one in 13 patients using this device. This excludes those
patients who had device embolisation following deployment (see
complications below). In total, 57 patients (96.6%) had complete
initial (pre-discharge) ductal closure using this device.
The dose–area product (DAP) in microgray units (
µ
Gy)
×
surface area/kg body weight was used to measure patient
radiation absorption. The median for this was 251
µ
Gym
2
/kg
(range: 85.5–679.4
µ
Gym
2
/kg) (Table 1).
35
With regard to complications, there were no patients who had
vascular injury, which might be because vascular access in all
infants less than 3 kg was via a size 4F vascular access sheath.
There were three patients with device embolisation (a major
complication). Two patients had devices (03x06L ADO II AS
and 04x06L ADO II AS) embolising into the right pulmonary
artery (RPA) and one (04x06L ADO II AS) into the left
pulmonary artery (LPA). All devices were retrieved with a size
10-mm (loop) AndraTec Exeter snare through a 4F AndraTec
introducer sheath (AndraTec GmbH, Simmernerstr, Koblenz,
Germany) (Fig. 3). It was easy to retrieve the device into the
sheath as it is a softer device compared to the ADO device.
The defect was closed with a larger ADO II AS device (05x06L
ADO II AS device) in one patient, closed with a 3.5
×
5-mm
Occlutech duct occluder device in another patient, and surgically
closed (off bypass) in the last patient. In addition, there were four
patients who required blood transfusion after the procedure. Of
these, three patients had haemoglobin levels of 11.7, 12.5 and 11.1
g/dl before the procedure. These levels decreased to 8.9, 9.7 and
10.1 g/dl, respectively, immediately after the procedure. The levels
improved to 14.5, 14.1 and 13.6 g/dl, respectively, following blood
transfusion. The fourth patient had excessive bleeding at the
puncture site following cardiac catheterisation. The haemoglobin
levels of this patient were 13.9 g/dl before, 8.2 g/dl immediatetly
after the procedure, and 13.2 g/dl following blood transfusion.
There were no complications after transfusion in these patients.
Minor complications involved two patients with bleeding at
the puncture site, which was managed conservatively. One patient
had catheter-induced supraventricular tachycardia before device
deployment, which was treated with a single dose of adenosine
at 100
µ
g/kg intravenously.
Concerning co-morbidity, one patient had a secundum atrial
septal defect, which measured 10 mm in diameter. It was
closed with a size 10.5-mm (waist) Figulla
®
Flex II Occlutech
septal occluder (Occlutech, Helsingborg, Sweden) at the age
Table 1. Demographics, haemodynamic and angiographic data of patients
Demographic, haemodynamic and angiographic data
Results, median (range)
Age, months
4 (0.8–7)
Weight at catheterisation, kg
3.6 (0.9–5.8)
Qp:Qs
2.4 (1.1–5.4)
Rp, Wood units
1.7 (0.3–7.12)
PA mean, mmHg
20 (9–47)
PDA narrowest diameter, mm
1.9 (1.0–3.4)
Ductal ampulla, mm
6.1 (2.8–10.6)
PDA length, mm
8.8 (3.7–18.4)
Descending aortic diameter, mm
5.3 (3.6–10.6)
Radiation exposure,
µ
Gym
2
/kg
251 (85.5–679.4)
Number of patients (
n
) and gender distribution:
n
=
59, F
=
32, M
=
27.
F, females; M, males; Qp, pulmonary blood flow; Qs, systemic blood flow; Rp,
pulmonary resistance; PA, pulmonary artery;
µ
Gym
2
/kg, microgray
×
square
meter surface area/kilogram body weight.



















