
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 1, January/February 2020
34
AFRICA
of congenital heart disease in the province of the Eastern Cape,
South Africa, it was used for the study, although the incidence of
PDA had not been documented there.
As part of the study protocol, the cohort included all those
patients who were under 6 kg at ductal closure, including
preterm infants, which included all those who were born before
37 weeks’ gestational age. Excluded from the study were patients
with other congenital heart diseases requiring surgery and those
that had severe congenital abnormalities with redirected overall
clinical care.
An echocardiographically haemodynamically significant PDA
(hsPDA) was defined as a PDA with a diameter of
>
1.4 mm/kg
body weight, with or without pulmonary hypertension, and a left
atrium:aortic ratio of
>
1.4:1.
27-29
Pulmonary hypertension was
defined as tricuspid regurgitation velocity of more than 3.4 m/s,
with an estimated pulmonary systolic pressure of more than 50
mmHg, with or without additional echocardiographic variables
suggestive of pulmonary hypertension.
29
The criteria for percutaneous closure of the PDA in the
premature infants involved in the study included those who
were diagnosed with an echocardiographically hsPDA that
had failed supportive therapy and medical treatment with anti-
prostaglandins (ibuprofen or paracetamol–indomethacin is not
used in our unit), and those who were ventilator-dependent and
required FiO
2
(fraction of inspired oxygen) of
>
60% after failed
supportive or medical therapy.
The criteria for ductal closure in other infants included
echocardiographic evidence of an hsPDA as above,
30
and signs
of left ventricular volume overload. In addition, the criteria
included those with severe pulmonary arterial hypertension with
pulmonary arterial pressures that were more than two-thirds of
systemic pressures or pulmonary vascular resistances that were
more than two-thirds of systemic vascular resistances, but still
with a left-to-right shunt and with pulmonary vascular reactivity
on vaso-reactive testing.
31
The study was conducted following clearance from the
Health Research and Bio-safety Committee of Walter Sisulu
University regarding Research in Human Subjects and from the
chief executive officer of Dora Nginza Hospital, Port Elizabeth.
Moreover, informed consent from patients’ parents or guardians
was obtained.
Prospective data collection and a review of records of
patients who had undergone percutaneous closure of a PDA
using the ADO II AS device in a single centre in South Africa
was performed. Due note was taken of the manufacturer’s
recommendation that this device should not be used for the
percutaneous closure of the PDA in patients who weigh less
than 6 kg. Moreover, the device is not FDA approved for routine
use in infants under 6 kg.
23
Parents were therefore informed
that, even though these devices are not FDA approved for
routine use in this weight group, they possess the Conformité
Européenne (CE) mark. This means that they may be utilised for
PDA closure in South Africa as per the South African Health
Products Regulatory Authority (SAHPRA) guidelines on the use
of medical devices in South Africa.
31,32
The patients’ age, gender and weight at the time of closure
were documented. Haemodynamic and angiographic data,
ductal morphology, device type and size, radiation exposure,
complications and outcomes were also recorded. The ductal
shape was classified using the Krichenko classification,
33
which
classifies ductal morphology according to five types. It is type A
if it is conical, B if it is tubular and less than 3 mm in length, type
C if it is tubular and more than 3 mm in length, D if it is complex
and has more than one constriction, and E if the duct is conical
and elongated. The descending aortic diameter was measured in
the thoracic aorta just distal to the PDA ampulla. A decision to
close a PDA using the ADO II AS was also based on a ductal
size of less than 4 mm, as per manufacturer’s guidelines. In
addition, associated congenital heart defects were documented.
In this study, values are reported as median (range). There
were no statistical comparisons that were required for this study.
In all treatment groups, an analysis of all complications
including events related to vascular access, sedation, airway and
cardiac catheterisation was done as described by Bergersen
et
al.
34
The complications were further classified as being ‘major’
or ‘minor’.
34
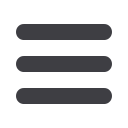
The ADO II AS device is made of a meshwork of self-
expandable nitinol wire. A detailed account of various device
sizes and guidelines regarding device selection for ductal closure
is documented by Kenny
et al
.
19
In brief, the device consists of
a central ‘lobe’, which measures 3–5 mm in diameter, and a
retention disk on each side of the lobe (Fig. 1). The disks are
1–1.5 mm more than the central lobe and range from 4–6.5
mm in diameter. The length of the device ranges from 2–6 mm.
The devices are delivered using a TorqVue low-profile delivery
system (4–5F) (Abbott Laboratories, St Jude Medical, St Marks,
Minnesota). ADO II AS transcatheter (percutaneous) delivery
protocol was adhered to.
19
During cardiac catheterisation, patients were sedated using a
mixture of intravenous midazolam (at 0.2 mg/kg) and ketamine
(at 2 mg/kg) as the initial dose, which was repeated as needed.
Femoral arterial and/or venous access was achieved using standard
4–5F vascular access short sheaths. In the premature infants and
infants where vascular access using standard vascular access set
with a 0.018-inch wire was a challenge, a 0.014-inch wire and a
21- or 23-gauge scalp vein set (Butterfly set) were used. Heparin,
at a dose of 50 U/kg, was given following femoral arterial access.
Fig. 1.
Amplatzer Duct Occluder type two additional sizes: the
device has two retention disks and a central lobe, and
is attached to a delivery wire. Published with permis-
sion from Abbott Laboratories, St Jude Medical, St
Marks, Minnesota.



















