
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 5, September/October 2020
264
AFRICA
Society of Echocardiography and the European Association of
Cardiovascular Imaging, a relative percentage decrease of GLS
>
15% (Fig. 3) compared with baseline and/or positive troponin
I levels during follow up will be considered subclinical ATRCD.
2
Only a few studies have reported the incidence of subclincal
ATRCD. Boyd
et al
.
15
used two-dimensional strain analysis
to detect subclinical LV systolic dysfunction in 140 breast
cancer patients early (within three month) after anthracycline
chemotherapy. Subclinical LV dysfunction (
>
11% reduction
in GLS) occurred in 22% of their patient cohort. In another
cohort of 159 patients receiving anthracycline, trastuzumab
(a monoclonal antibody for treating HER2 receptor-positive
breast cancer) or both,
16
decreased GLS (by
>
11%) was found
in 33% of patients seven months after the completion of the
chemotherapy treatment. Interestingly, LVEF remained within
normal ranges in both studies.
African populations who are at risk of
developing ATRCD
Cancer is emerging as a major public health problem in
sub-Saharan Africa (SSA) because of population aging and
growth, as well as increased prevalence of key risk factors,
including those associated with social and economic transition.
A high residual burden of infectious agents (HIV/AIDS, human
papillomavirus, hepatitis B virus) in certain SSA countries
unquestionably drives the rates of certain cancers. Indeed, about
one-third of all cancers in the region are estimated to be infection
related.
17
Breast and cervical cancer in women and prostate
cancer in men are the major cancers with a poor outcome in
SSA.
17
The growing prevalence and pattern of cancer in SSA
determine the large role of anthracycline in cancer treatment
in SSA. In the developed world, anthracycline has been used
much less frequently, being partially replaced by novel, less
cardiac-toxic anti-tumour drugs when treating certain types of
cancer.
18
However, most of these novel drugs are costly and so
not available in SSA.
Following the launching of the African Cancer Network
Project in 2012, more than 100 cancer treatment institutions were
set up by 2015.
19
More and more African cancer patients are able
to receive anthracycline-based chemotherapy. Although there
are no reliable data on how many patients are receiving these
anti-tumour drugs in Africa, it has been estimated that about
60% of cancer patients in the Uganda Cancer Institute (UCI)
are treated with anthracycline. The common cancers treated
with anthracyclines at UCI include breast cancer (68.75%),
non-Hodgkin’s lymphoma (13.13%), Hodgkin’s lymphoma
(5.6%), advanced hepatocellular cancer (3.7%), soft tissue
sarcomas (3.7%) and leukaemia (3.1%). Moreover, 80% of this
population that are at risk of cardiotoxicity are women.
17
Association of anthracycline cardiotoxicity
risk with ethnicity and gender
Studies investigating sexual dimorphism of anthracycline
cardiotoxicity are sparse. Yet growing evidence, mainly obtained
in experimental studies, pinpoints a sexual dimorphism of
doxorubicin cardiotoxicity, with females being protected
compared to males.
20
This protection includes the essential
targets of anthracycline, that is energy metabolism, energetic
signalling pathways and oxidative stress.
20
In a review article of anthracycline cardiotoxicity in
childhood cancer survivors, Armstrong
et al
.
21
identified 17
studies evaluating gender as a risk factor for cardiotoxicity
after anthracyclines and found five, including four high-quality
studies, to validate that females experienced a poorer outcome
than males. It has been suggested that doxorubicin cardiotoxicity
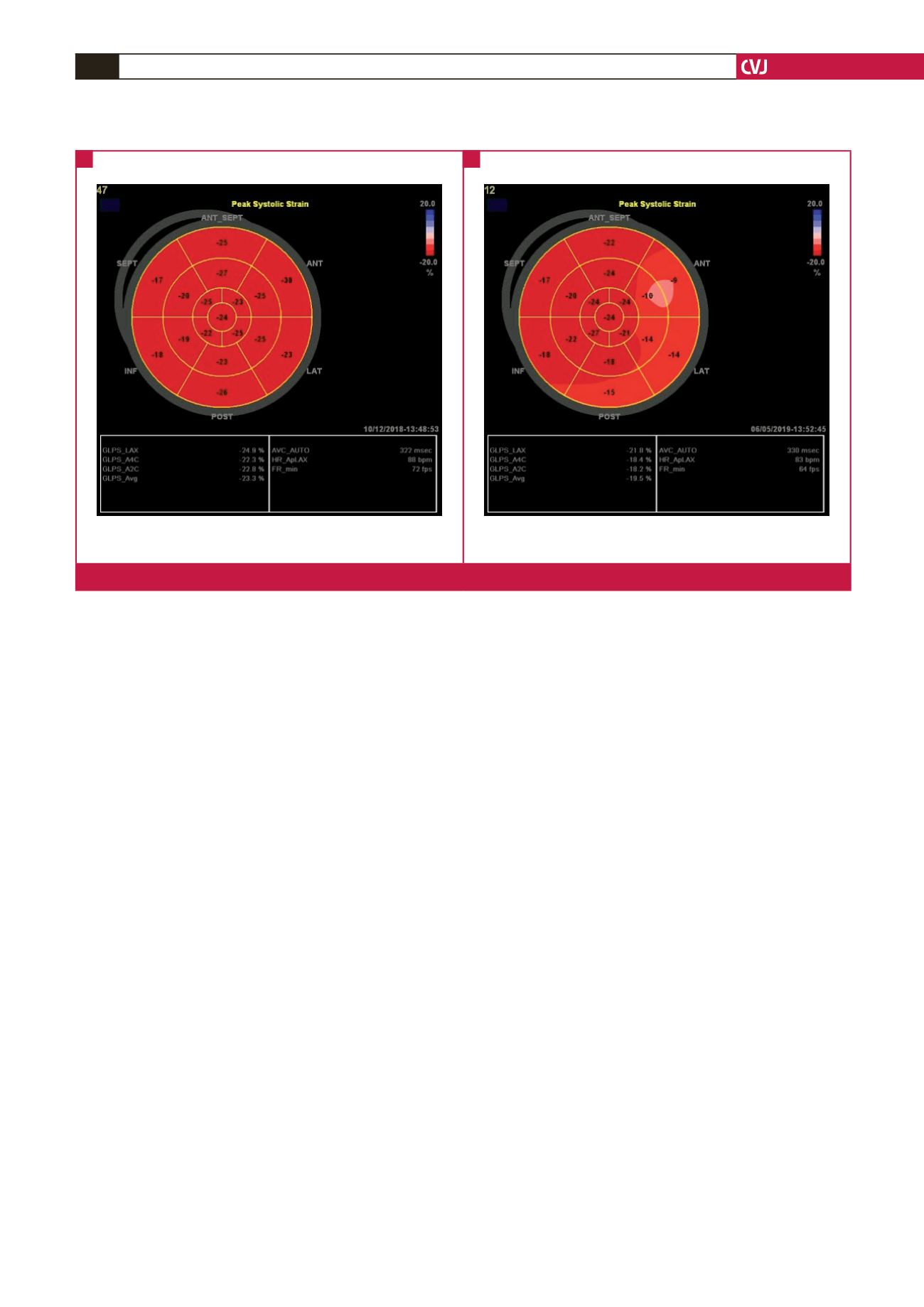
Baseline
GLS: –23.3%
EF: 66%
Completion of anthracycline therapy
GLS: –19.5%
EF: 57%
Fig. 3.
Strain images of a patient who was diagnosed with subclinical ATRCD by GLS.
A
B



















