
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 6, November/December 2020
AFRICA
287
of lower-extremity DVT, and to compare its efficacy in subjects
with acute and subacute DVT.
Methods
This single-arm, prospective study was conducted on patients
with acute (
<
15 days) or subacute (15–30 days) DVT who
underwent PMT in a tertiary centre between September 2017
and September 2019. Written informed consent was obtained
from all participants. The study was approved by the institutional
review board and was performed in accordance with the most
recent version of the Helsinki Declaration. The study was
prospectively registered at clinicaltrials.gov.
Inclusion criteria were as follows: age between 18 and 75 years,
having suffered from an iliofemoral or femoropopliteal DVT
within the last 30 days, and receiving duplex ultrasonography
imaging. Subjects with any absolute contra-indications for
thrombolytics, previous contrast allergy, pregnancy, malignancy
requiring chemotherapy, those within less than 14 days of
surgery, and those with a creatinine clearance rate
<
50 ml/min
were also excluded.
DVT of the lower limb was confirmed with duplex
ultrasonography. Baseline fibrinogen and D-dimer levels were
measured in all subjects. All subjects received anticoagulation
with unfractionated heparin from admission to discharge.
With ultrasonographic guidance, a 6F sheath was placed
into the contralateral femoral vein under local anaesthesia.
Temporary inferior vena cava (IVC) filters (Reya Venocat,
Biolas, Ankara, Turkey) to the infrarenal IVC were deployed in
all patients under fluoroscopic guidance to prevent the risk of
clot-fragment embolisation during the procedure. The patient
was then placed in the supine position and ultrasonography was
used to enter the popliteal vein on the side of the DVT using a 6F
sheath. A pre-interventional venogram was obtained to evaluate
the location and severity of the thrombus.
A 0.018-inch hydrophilic guidewire (Terumo glidewire, NJ,
USA) was used to traverse the thrombotic lesion, followed by
the advancement of a catheter with multiple side holes (UniFuse
Infusion Catheter; Angiodynamics, Latham, NY, USA) through
the guidewire. Doses of 200 000 IU of urokinase were then
administered into the occlusion through the multi-hole catheter
for 15 to 20 minutes. Control venography was performed to
assess venous flow and rate of recanalisation. Percutaneous
balloon dilatation and stent placement (Jaguar, Balton Co,
Warsaw, Poland) were carried out in cases with residual iliac vein
stenosis of over 50%. An aspiration catheter was used to aspirate
any remaining residual thrombus.
The IVC filter was retrieved after thrombolysis under
fluoroscopic guidance (Fig. 1). Following thrombolysis, subjects
were kept on unfractionated heparin, and rivaroxaban (Xeralto)
20 mg/day was initiated and maintained for 12 months. All
study subjects underwent a ventilation–perfusion (VQ) scan
for detection of the pulmonary embolism during the follow
up. All subjects were recommended to use knee-high, elastic
compression stockings for 24 months.
Subjects were categorised according to the degree of
post-interventional recanalisation as follows: (1) complete
recanalisation if the length of the residual thrombus was
<
2
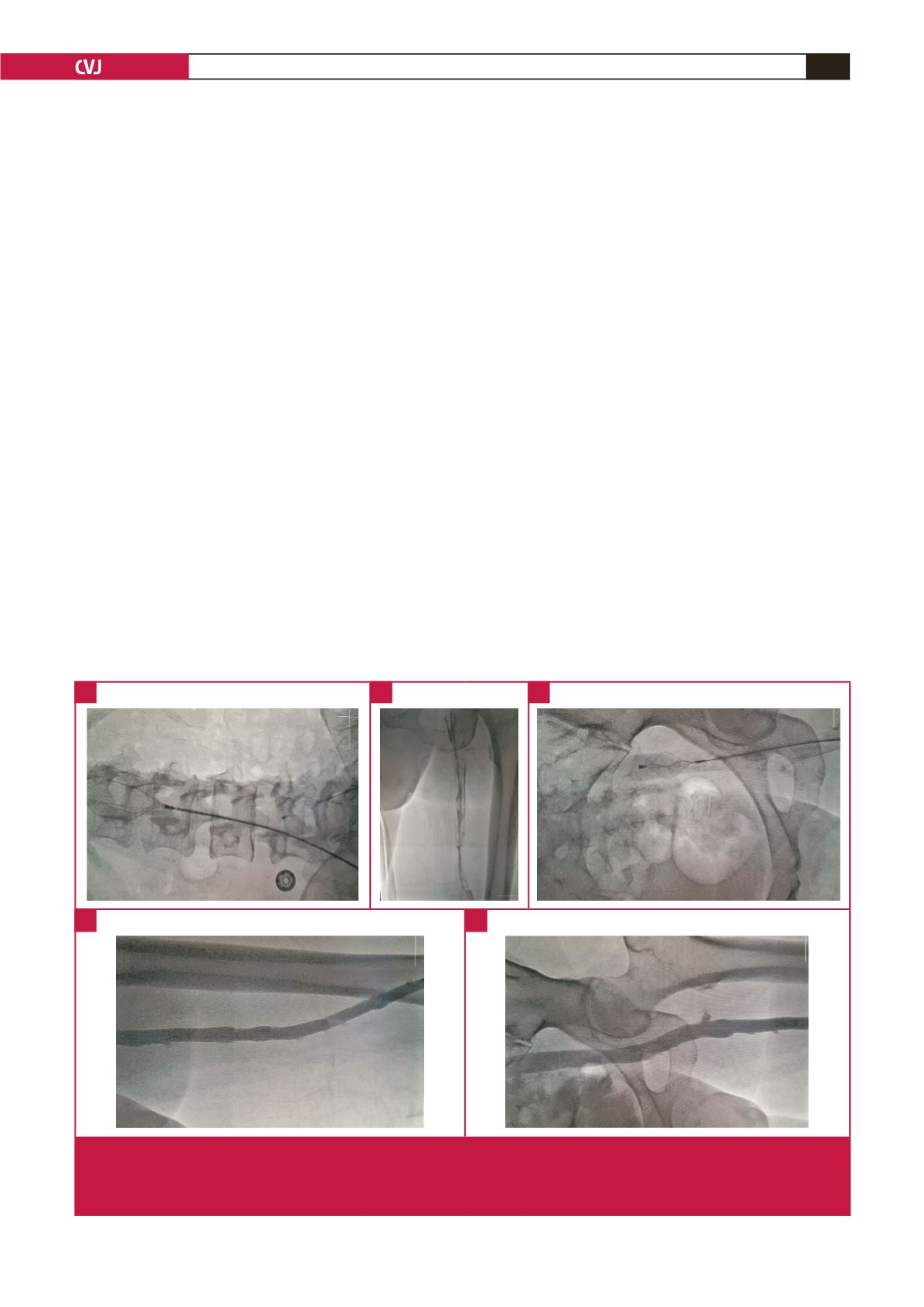
Fig. 1.
A: Temporary inferior vena cava (IVC) filters were deployed in all patients to the infrarenal IVC under fluoroscopic guidance
to prevent the risk of clot-fragment embolisation during the procedure. B: Entering the popliteal vein on the side with the DVT
using a 6F sheath. C: Urokinase was administered into the occlusion through the multi-hole catheter for 15 to 20 minutes. D:
Femoropopliteal recanalised venous flow. E: Iliofemoral recanalised venous flow.
A
D
E
B
C



















