
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 6, November/December 2020
288
AFRICA
cm and venous flow was not limited; (2) partial recanalisation
if the length of the residual thrombus was
>
2 cm and venous
flow was slightly limited by the residual thrombus; (3) poor
recanalisation if the venous flow was prominently limited by the
residual thrombus. Interventional complications were classified
as minor (epistaxis, haematuria, skin ecchymosis) and major
complications (pulmonary embolus, intracranial haemorrhage
and major bleeding requiring blood transfusion).
All subjects underwent control duplex ultrasonography to
evaluate the patency of the relevant vein. Fibrinogen and
D-dimer levels were also re-measured. The percentage of vessel
patency and PTS development in the third month after PMT
were the primary outcome measures of this study.
Statistical analysis
All analyses were performed on SPSS v20 (IBM, Armonk, NY,
USA). The Shapiro–Wilk test was used for the normality check.
Data are presented as mean
±
standard deviation or median
(minimum–maximum) for continuous variables, with regard
to normality. Comparison of the pre- and post-thrombolysis
fibrinogen and D-dimer levels was performed with the paired
samples
t
-test. A two-sided
p
<
0.05 was accepted as statistically
significant.
Results
A total of 35 subjects (mean age 62
±
14 years, 57% male) with
lower-extremity DVT who underwent PMT were enrolled in
this study. Baseline characteristics of the study population are
presented in Table 1; 57% of the cases were acute DVT (
<
15
days) and 77% were in the femoropopliteal region. More than
half of the cases were unprovoked DVT.
Complete recanalisation was noted in 23 subjects (66%),
whereas recanalisationwasdefinedaspoor in two (6%).Aspiration
thrombectomy was performed as adjunctive technique to remove
the residual thrombus in two subjects with poor recanalisation
and in seven subjects with partial recanalisation after catheter-
directed thrombolysis (CDT). Two patients in the subacute DVT
group received stents for residual iliac vein stenosis.
The rate of minor complications was 14%. None of the
subjects experienced major complications such as intracranial
haemorrhage or pulmonary embolism. No mortality was
recorded during the three months of follow up. Control duplex
ultrasonography in the third month revealed that the target veins
were patent in all subjects. None of the subjects experienced PTS
during the three months of follow up.
Comparison of the subjects with acute and subacute DVT is
given in Table 2. Subjects with subacute DVT were older than
those with acute DVT (70
±
11 vs 56
±
14 years,
p
=
0.003).
There were no significant differences between subjects with
acute and subacute DVT in terms of risk factors for DVT,
aetiology, baseline and third-month fibrinogen and D-dimer
levels. Although the frequency of minor complications was
slightly higher in those with subacute DVT, the difference did
not reach statistical significance. The percentage of patients with
acute complete recanalisation was significantly higher in those
with acute DVT compared to those with subacute DVT (95 vs
27%,
p
<
0.001).
Discussion
This study aimed to investigate the role of PMT with low-dose
urokinase in patients with acute or subacute lower-extremity
DVT. Our findings demonstrate that PMT with low-dose
urokinase not only provided excellent vessel patency at three
months but also enabled safe thrombolysis due to the delivery of
lower-dose agents into the thrombus. Notably, with this method,
the acute complete recanalisation rate was significantly higher in
subjects with acute DVT than those with subacute DVT.
The main therapeutic goals for treating lower-extremity
DVT are the preservation of venous valve function and
prevention of pulmonary embolism and recurrent DVT.
Systemic anticoagulation with low-molecular weight heparin
or unfractionated heparin followed by warfarin or new oral
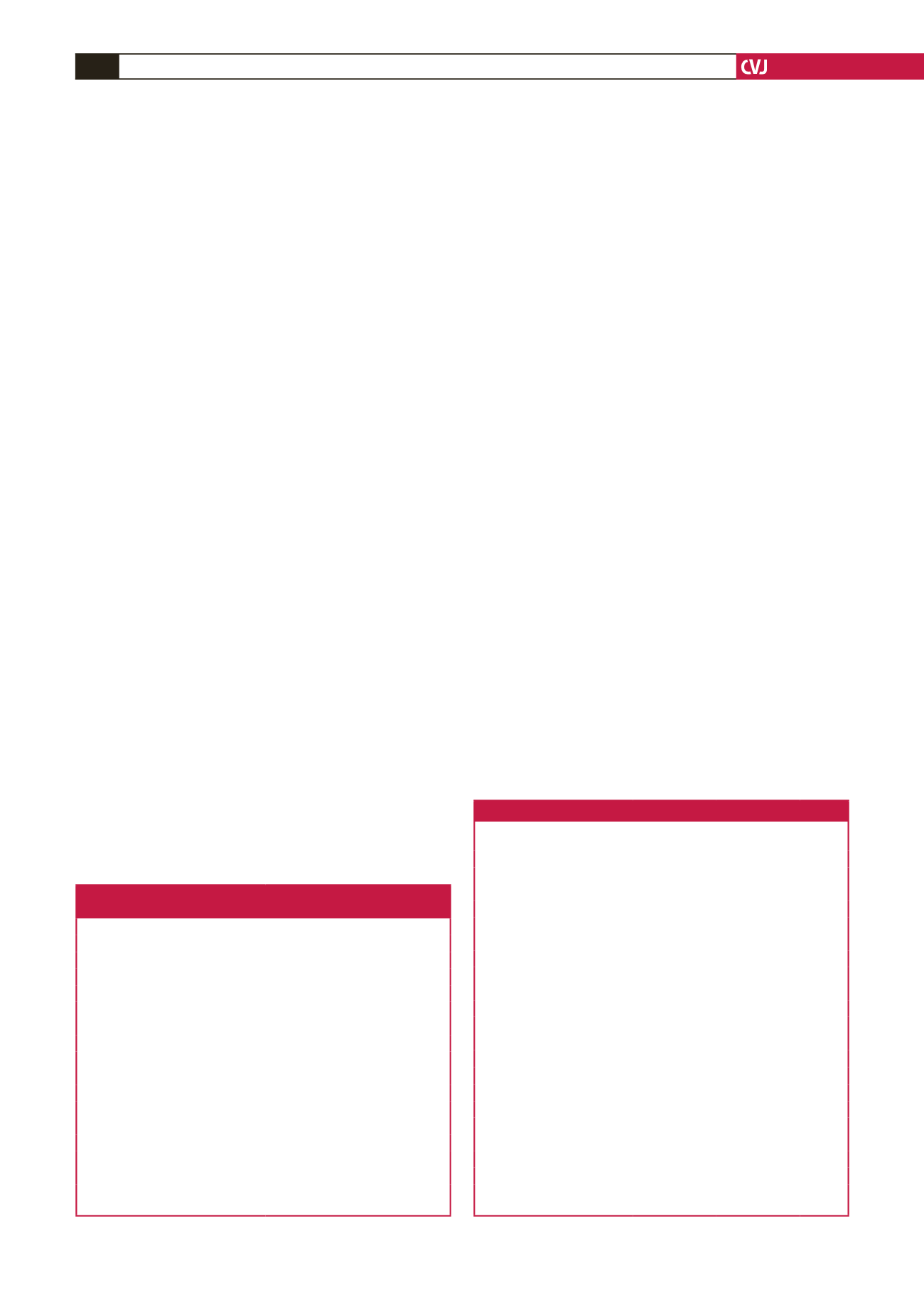
Table 1. Demographic features and clinical characteristics
of the study population (
n
=
35)
Demographic features
Number (%)
Age, years
62
±
14
Gender, male
20 (57)
Acute DVT
20 (57)
Location
Iliofemoral
8 (23)
Femoropopliteal
27 (77)
Diabetes
8 (23)
Dyslipidaemia
6 (17)
Smoking
13 (37)
Coronary artery disease
4 (11)
Aetiology
Major surgery
3 (9)
Obstetric conditions
4 (11)
Prolonged immobilisation
8 (23)
Unprovoked
20 (57)
Data are presented as mean
±
standard deviation for continuous variables and
frequency (%) for categorical variables.
Table 2. Comparison of subjects with acute and subacute DVT
Acute DVT
(n
=
20) n (%)
Subacute DVT
(n
=
15) n (%) p-value
Age, years
56
±
14
70
±
11
0.003
Gender, male
11 (55)
9 (60)
0.767
Dyslipidaemia
4 (20)
2 (13)
0.605
Diabetes
3 (15)
5 (33)
0.201
Coronary artery disease
2 (10)
2 (13)
0.759
Smoking
8 (40)
5 (33)
0.686
Aetiology
0.254
Major surgery
3 (15)
0 (0)
Obstetric conditions
3 (15)
1 (7)
Prolonged immobilisation
3 (15)
5 (33)
Unprovoked
11 (55)
9 (60)
Baseline fibrinogen (mg/dl)
472
±
114
425
±
99
0.214
Fibrinogen at 3rd month (mg/dl)
355
±
85
304
±
83
0.088
Baseline D-dimer (µg/ml)
3.4
±
1.2
4.2
±
2.4
0.287
D-dimer at 3rd month (µg/ml)
1.1
±
0.6
1.8
±
1.1
0.232
Complete recanalisation
19 (95)
4 (27)
<
0.001
Partial recanalisation
1 (5)
9 (60)
Poor recanalisation
0
2 (13)
Minor complications
1 (5)
4 (27)
0.070
Patency at 3rd month
20 (100)
15 (100)
>
0.999
Data are presented as mean
±
standard deviation for continuous variables and
frequency (%) for categorical variables.



















