
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 1, January/February 2021
18
AFRICA
DDDR pacing, reported a higher incidence of paroxysmal AF
with AAIR pacing compared to DDDR pacing, with a high risk
of complications with subsequent pacemaker lead revisions.
6
This study aimed to compare the outcomes (development of
AF, AV block, lead revision and device sepsis) of AAIR versus
DDDR pacing in patients with symptomatic SND using AV
nodal functional testing at the time of implant (patients received
DDDR pacing if there was evidence of AV Wenkebach or AV
block with atrial pacing at 120 bpm).
The rationale for using AV nodal functional testing was
based on a previous observational study that compared AAIR
versus DDDR pacing with very long-term follow up. The
authors reported that AV nodal functional testing using a
Wenkebach block point lower than 120 bpm was found to be a
predictor of later high-grade AV block.
7
Patients also received
a DDDR pacemaker if there was evidence of bundle branch
block (BBB) or AV block (except 1st degree AV block and
fascicular blocks) at baseline. While the risk of development of
AV block in patients with BBB remains unclear, the decision to
implant a pacemaker is consistent with the DANPACE trial.
A previous study reported an increase in cardiovascular death
rate in patients with BBB, which may be related to the future
development of AV block.
14,15
Methods
A retrospective study was conducted on consecutive patients
implanted with an AAIR or DDDR pacemaker for symptomatic
SND at Groote Schuur Hospital (GSH) between 2007 and 2017.
GSH is a large, government-funded teaching hospital in Cape
Town, South Africa. GSH is a tertiary referral centre, based on
a networking hub with secondary hospitals in the region, and
therefore the recruited patients are representative of the general
population.
Ethics approval was obtained from the Faculty of Health
Sciences Human Research Ethics Committee of the University
of Cape Town (UCT), HREC REF: 493/2017.
Clinical records were obtained from cardiologists’ and cardiac
technologists’ implant records and patients’ hospital files. All
patients with a diagnosis of SND who received a pacemaker were
included. Demographic and clinical variables were recorded on
a clinical report form.
Socio-demographic variables including age, gender,
presenting symptoms, co-morbidities, medications, ECG and
echocardiographic findings were retrieved. Other parameters
obtained were the mode of pacing and outcomes after pacing,
including occurrence of complications such as the development
of AF, AV block, lead revision and device sepsis.
Statistical analysis
The collected data were checked for quality and coding was
done prior to entry. Two different people entered the data twice
and checked to ensure no double or wrong entries. Continuous
and discrete data are presented as mean ± SD and as counts
(percentage), respectively. All mean ages reported were calculated
at primary implantation. The Statistical Package for the Social
Sciences 24.0 (SPSS, Inc, Chicago, IL, USA) for Windows was
used. The chi-squared test was used to test for group differences
at
p
< 0.05 significance level.
Results
A total of 211 patients received a permanent pacemaker between
January 2007 and July 2017 at GSH. One hundred and sixteen
patients (54.9%) received a pacemaker for symptomatic SND, 54
(46.6%) received an AAIR pacemaker and 62 (53.4%) a DDDR
pacemaker based on BBB, AV block at baseline and AV nodal
functional testing (Table 1).
A comparison of the baseline demographics, clinical
presentation and co-morbidities of the patients who received
AAIR and DDDR pacemakers is shown in Table 1. Overall,
the majority (66.4%) of patients was female and symptomatic,
with pre-syncope or syncope being the most common clinical
presentation (84.4%). Patients in theDDDRgroupwere alsomore
likely to have experienced palpitations at presentation (22.6%,
p
= 0.05). There were no major differences in co-morbidities
(hypertension, diabetes mellitus, renal disease, cerebrovascular
disease, ischaemic heart disease) between the two groups.
The ECG subgroups of sinus node dysfunction are shown
in Table 2. Patients who received DDDR pacing had a higher
likelihood of having BBB (6.5%) and evidence of AV block
(24.2%) at baseline. There were no significant differences in ECG
categories of SND (sinus bradycardia, sinus pauses/arrest, sino-
atrial exit block, tachy–brady syndrome) between the AAIR and
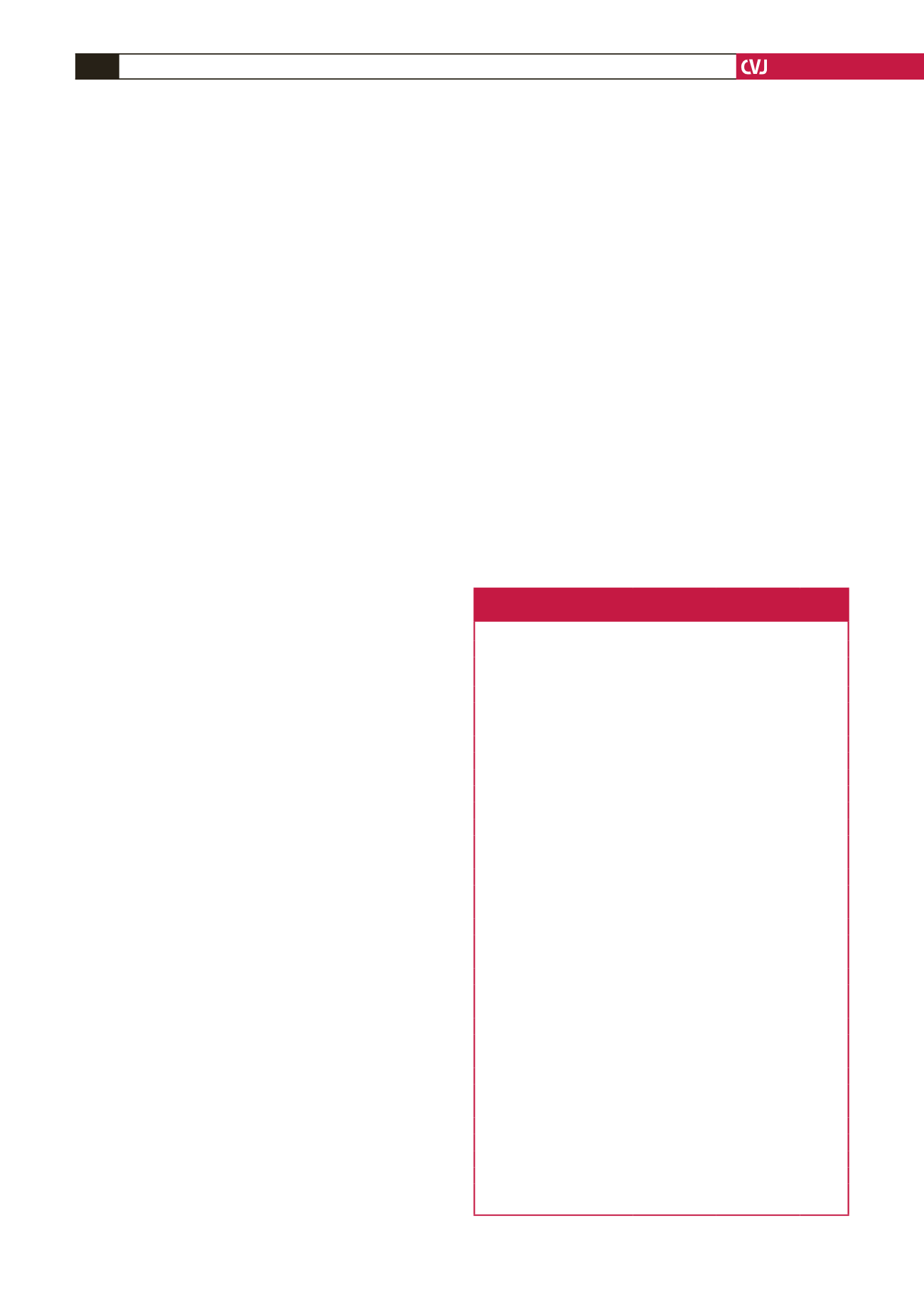
Table 1. Baseline demographics and clinical presentation of patients
who received AAIR versus DDDR pacing for sinus node dysfunction
Characteristic/parameter
AAIR (n = 54) DDDR (n = 62)
p
-value
Females,
n
(%)
38 (70.4)
39 (62.9)
0.396
Age at first implantation,
mean ± SD (years)
65.8 ± 15.2
65.0 ± 15.4
0.766
Pre-syncope/syncope,
n
(%)
Yes
45 (83.3)
53 (85.5)
0.750
No
9 (16.7)
9 (14.5)
Tiredness,
n
(%)
Yes
23 (42.6)
27 (43.5)
0.917
No
31 (57.4)
35 (56.5)
Dizziness,
n
(%)
Yes
44 (81.5)
54 (87.1)
0.405
No
10 (18.5)
8 (12.9)
Palpitations,
n
(%)
Yes
5 (9.3)
14 (22.6)
0.053
No
49 (90.7)
48 (77.4)
Heart failure,
n
(%)
Yes
2 (3.7)
4 (6.5)
0.684
No
52 (96.3)
58 (93.5)
Hypertension,
n
(%)
Yes
41 (75.9)
41 (66.1)
0.248
No
13 (24.1)
21 (33.9)
Diabetes mellitus,
n
(%)
Yes
18 (33.3)
17 (27.4)
0.489
No
36 (66.7)
45 (72.6)
Renal disease,
n
(%)
Yes
2 (3.7)
4 (6.5)
0.684
No
52 (96.3)
58 (93.5)
Cerebrovascular events,
n
(%)
Yes
5 (9.3)
4 (6.5)
0.732
No
49 (90.7)
58 (93.5)
Ischaemic heart disease,
n
(%)
Yes
24 (44.4)
27 (43.5)
0.923
No
30 (55.6)
35 (56.5)
AAIR: atrial-pacing atrial-sensing inhibited-response rate-adaptive; DDDR:
dual-pacing dual-sensing dual-response rate-adaptive.



















