
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 2, March/April 2021
AFRICA
81
Tosilizumab, an IL-6 antagonist, was added in addition
to other treatments in patients who developed macrophage
activation syndrome findings with worsening of pneumonia and
acute-phase response.
Tosilizumab was used in patients with severe pneumonia and
serum CRP level
>
70 mg/l and serum ferritin level
>
1 000 ng/
ml, and also if there were at least two of the following criteria:
•
fever (
≥
38.5°C)
•
hepato/splenomegaly
•
bicytopaenia /pancytopaenia
•
triglycerides
>
350 mg/dl (3.96 mmol/l)
•
fibrinogen
<
250 mg/dl
•
aspartate aminotransferase
>
42 U/l
•
haemophagocytosis in the bone marrow
•
immunosuppression.
Statistical analysis
Descriptive statistics were obtained for all study data. Categorical
variables were compared for the study outcome using the Fisher
exact test or
χ
2
test, and continuous variables were compared using
the
t
-test or the Mann–Whitney
U
-test, as appropriate. Variables
were investigated using visual (histograms, probability plots) and
analytical methods (Kolmogorov–Simirnov/Shapiro–Wilk’s test)
to determine whether they were normally distributed. Continuous
data are expressed as mean (SD) or median [interquartile range
(IQR)] values. Categorical data are expressed as proportions.
The Pearson correlation coefficient and Spearman rank
correlation coefficient were used for linear correlation analysis.
The ANOVA test was used to compare laboratory findings of
patients grouped according to thorax computerised tomography
(CT) scans. The Bonferroni test was used for
post hoc
analysis
of the multiple comparisons. Data were analysed using SPSS
version 25.0 (IBM). A two-sided
p
<
0.05 was considered
statistically significant. Analysis began on 11 April 2020.
Results
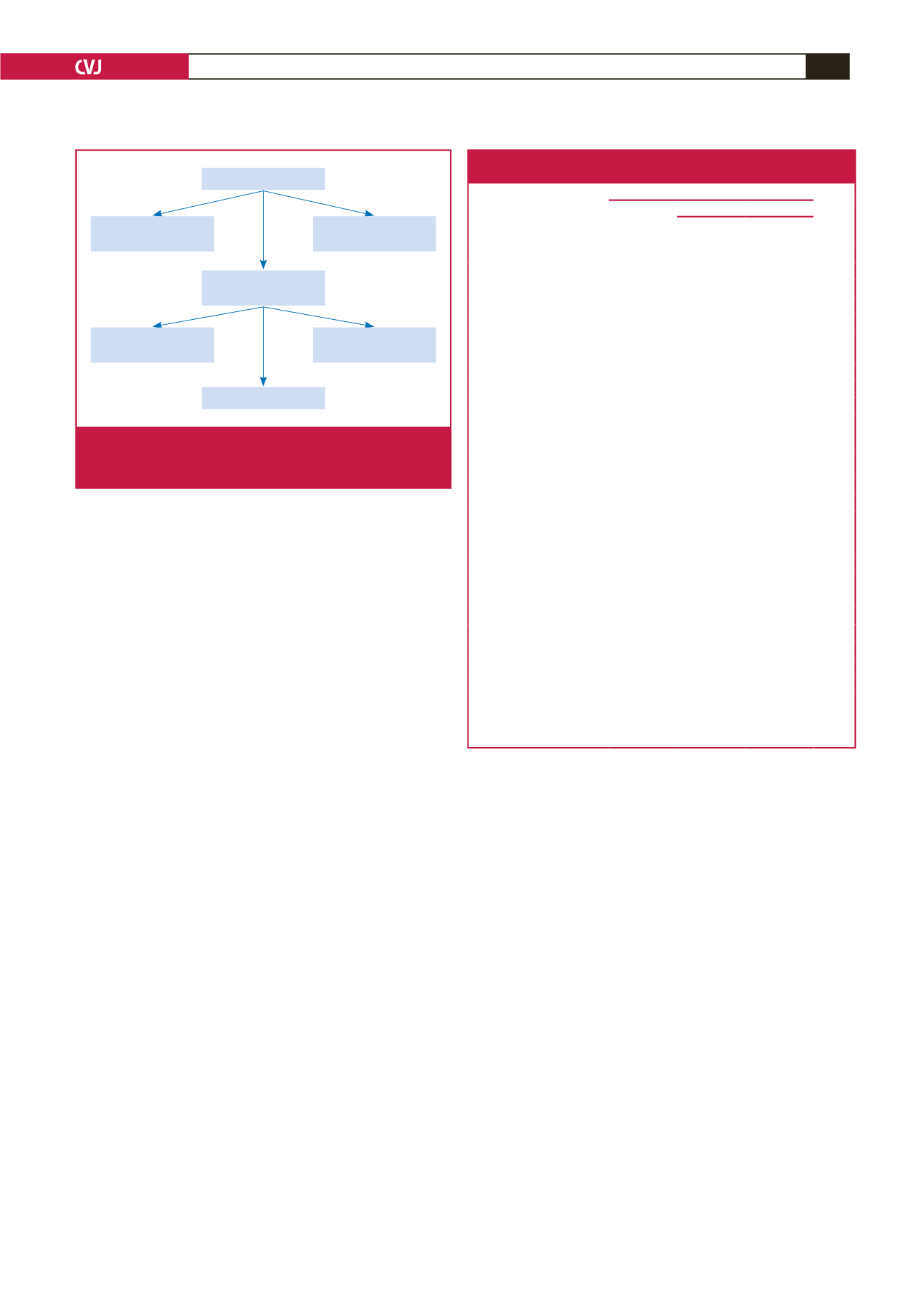
Patients admitted to the COVID wards (309 patients) between
11 March and 10 April were included in the study. During this
period, a total of 32 patients were taken to the ICU. Ten of
these ICU patients died and six were discharged. The intensive
care treatments of the remaining 16 patients were ongoing. Our
mortality rate was 3%. A total of 154 patients hospitalised in the
COVID wards were discharged. Treatment of the remaining 123
patients is ongoing (Fig. 1).
Baseline characteristics, signs, symptoms, accompanying
chronic diseases and drug usage of the patients are shown in
Table 1. The median age of the study population was 57 years
(23–94). There was a statistically significant difference between
the median ages of patients with and without cardiac injury
(
p
<
0.001) (Table 1). The study population was slightly male
predominant (61%) but it was not statistically significant (
p
>
0.05) (Table 1).
Unpredictably, the proportion of smokers was statistically
significantly lower in patients with myocardial injury than in
those without injury (
p
<
0.01) (Table 1).
It was only shortness of breath that reached statistical
significance in terms of the symptoms of patients with and
without cardiac damage at the time of hospitalisation (
p
<
0.001)
(Table 1).
Saturations and respiratory rates were statistically significantly
different when patients with and without cardiac damage were
compared in terms of vital signs at the time of admission (
p
<
0.001) (Table 1).
Table 1. Baseline characteristics, signs, symptoms, accompanying
chronic diseases and drug usage of the patients
Patients, n (%)
Cardiac injury
p-value
Characteristics
All
(n
=
309)
With
(n
=
78)
Without
(n
=
231)
Age, median (range), years
57 (23–94)
70 (32–94)
52 (23–93)
<
0.001
Males
190 (61)
46 (59)
144 (62)
>
0.05
Smoking
49 (16)
4 (5)
45 (19)
<
0.01
Signs and symptoms at admission
Fever
241 (78)
48 (61)
193 (83)
>
0.05
Cough
279 (90)
68 (87)
211 (91)
>
0.05
Sputum production
12 (3)
3 (3)
9 (3)
>
0.05
Shortness of breath
111 (36)
45 (58)
66 (28)
<
0.001
Fatigue
298 (91)
73 (93)
225 (97)
>
0.05
Nausea
47 (15)
10 (12)
37 (16)
>
0.05
Diarrhoea
21 (6)
3 (3)
18 (7)
>
0.05
Anosmia
14 (4)
1 (1)
13 (5)
>
0.05
Saturation, median (range),
%
94 (79–99)
91 (79–98)
95 (82–99)
<
0.001
SBP, median (range), mmHg 130 (80–200) 132 (80–200) 128 (80–180)
>
0.05
DBP, median (range), mmHg 75 (50–120) 75 (50–120) 76 (50–110)
>
0.05
Pulse, median (range), bpm 94 (50–123) 94 (50–123) 94 (52–122)
>
0.05
RR, median (range), breaths/
min
18 (14–34)
23 (14–34)
19 (14–32)
<
0.001
Chronic disease/ACEI/ARB usage
Hypertension
122 (39)
53 (67)
69(30)
<
0.001
CAD
33 (11)
21 (27)
12 (5)
<
0.001
CHF
18 (6)
15 (19)
3 (1)
<
0.001
COPD
32 (10)
15 (19)
17 (7)
<
0.01
Diabetes
69 (22)
24 (31)
45 (19)
0.02
CKD
43 (14)
26 (33)
17 (7)
<
0.001
ACEI/ARB usage
78 (25)
30 (38)
48 (21)
>
0.05
SBP, systolic blood pressure; DBP, diastolic blood pressure; RR, respiratory
rate; CAD, coronary artery disease; CHF, chronic heart failure; COPD, chronic
obstructive pulmonary disease; CKD, chronic kidney disease; ACEI, angiotensin
converting enzyme inhibitor; ARB, angiotensin receptor blocker.
32 patients admitted
to ICU department
309 patients
154 patients recovered
and discharged
123 patients
still on treatment
6 patients recovered
and discharged
16 patients still
on treatment
10 patients died
Fig. 1.
Flowchart of the patients admitted to the COVID-19
wards (309 patients) between 11 March and 10 April
2020 and included in the study.



















